Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Autoimmune/autoinflammatory Pigmentary disorders
Author: Dr Bushra Alsayaydeh, Dermatologist, Amman, Jordan, August 2022. Previously: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1999.
Introduction
Demographic
Causes
Clinical features
Classification
Severity assessment
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outcome
Vitiligo is an acquired, chronic, depigmenting disorder of the skin, in which pigment-producing cells (melanocytes) that determine the colour of skin, hair, and eyes are progressively lost. It appears as milky-white patches of skin (leukoderma) and can be cosmetically very disabling, particularly in people with dark skin.
It is currently widely accepted that vitiligo is the result of autoimmune destruction of melanocytes.

Vitiligo over the knuckles - keobnerisation due to trauma often localises vitiligo

Symmetrical wrist vitiligo - a common location (V-patient1)

Vitiligo over the back and elbows

Vitiligo on the lid with poliosis of the lashes
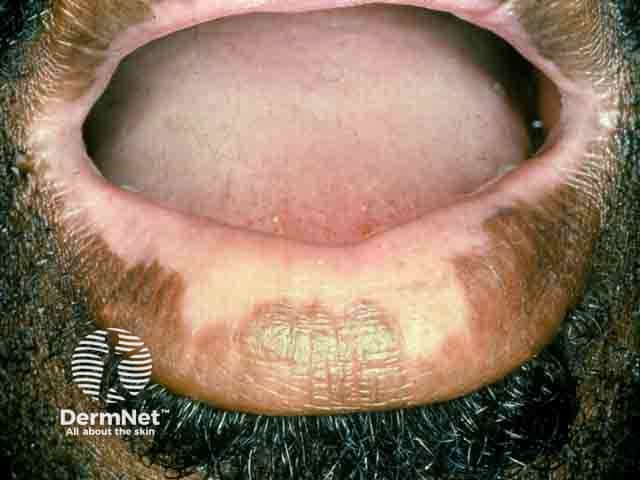
Vitiligo on the lips

Follicular repigmentation in a patch of vitiligo

Extensive symmetrical facial vitiligo

Vitiligo around the hairline of a Samoan woman (V-patient3)
Click here for more images of vitiligo
Vitiligo affects 0.5–2% of the population.
Autoimmune disease development has been associated with generalized vitiligo, the most common type of vitiligo, especially if there is a family history of vitiligo and other autoimmune disorders.
Vitiligo is also three times more common in recipients of allogeneic bone marrow and stem-cell transplants than in the healthy population.
Vitiligo is due to the loss or destruction of melanocytes (melanin-producing cells).
Genetic factors appear to contribute to 80% of vitiligo risk, whilst environmental factors account for 20%. Many genetic loci have been identified, all related to the immune system, except for TYR which encodes tyrosinase, a key enzyme in melanin production and a major autoantigen in vitiligo.
The convergence or integrated theory combines immunological, biochemical, oxidative, and environmental mechanisms that work jointly in those with a genetic susceptibility is widely accepted.
This could be explained through three phases:
Understanding the molecular pathogenesis of vitiligo serves as a promising source for the development of more targeted therapies.
Vitiligo is also a component of some rare multiorgan syndromes, such as:
These syndromes affect organs that normally house melanocytes, and are now believed to constitute one disease entity with variable clinical expression.
Other rare dermatologic syndromes that present with lesions indistinguishable from vitiligo are:
A vitiligo-like leukoderma may occur in patients with metastatic melanoma.
Vitiligo can also be induced by drugs, such as immune checkpoint inhibitors (pembrolizumab, nivolumab) and BRAF inhibitors (vemurafenib, dabrafenib) used to treat metastatic melanoma.
The onset of vitiligo is usually insidious.
The most common presentation is the complete loss of pigment in single or multiple macules or patches of skin, with characteristic chalk- or milky-white colour.
Severity is variable and there is no way to predict how much or how fast pigment will be lost.
For more information, see the section on severity assessment below.
The Vitiligo European Task Force (VETF) came to a consensus about the classification of vitiligo in 2007. They decided on four main categories with subtypes.
Classification |
Subtypes |
Comments |
Non-segmental vitiligo |
|
|
Segmental vitiligo |
|
|
Mixed vitiligo |
|
|
Unclassified vitiligo |
|
|
More than 90% of the adult vitiligo cases are of the generalized vulgaris or acrofacial types, while in children, segmental vitiligo constitutes 15–30% of the cases.
Rare clinical subtypes of vitiligo include:
Click here for images of vitiligo
In most cases, the severity of vitiligo is not formally assessed. However, clinical photographs may be taken to monitor the condition.
At least two scoring systems have been devised for vitiligo and are used in clinical trials.
VASI is based on the PASI scoring system for psoriasis. It measures the extent and degree of depigmentation in 6 sites: hands, upper extremities, trunk, lower extremities/feet, and the head and neck.
VETF is based on SCORAD scoring system for atopic dermatitis. The VETF assesses the extent, staging, and spreading/progression in 5 sites: head/neck, trunk, arms, legs and hands/feet. It grades from 0 (normal pigmentation) to 4 (complete hair whitening). Spreading is assessed using the following scores: 0 (stable disease), -1 (regressive disease) and +1 (progressive disease).
VETF includes a clinical assessment form to record the sex, age, duration of disease, age of onset, episodes of repigmentation, the impact of vitiligo on quality of life, family history, additional medical conditions, and the Fitzpatrick skin type of the patients.
The distribution and characteristics of vitiligo patches are similar in different skin types; however, while vitiligo can be barely noticeable in some people with lighter skin complexions, it is usually more obvious in darker skin types. This can cause significant cosmetic disability, along with its psychological consequences.
Vitiligo has an otherwise benign nature with most of those affected being in good health.
Vitiligo is usually a clinical diagnosis, based on its characteristic appearance, and no specific tests are required to make the diagnosis.
Tools that can aid in diagnosis include:
Blood tests
There is no cure for vitiligo and treatment is often unsatisfactory. The aim is to stop progression of the disease (stabilisation), and to achieve satisfactory re-pigmentation.
Treatment is most successful on the face and trunk; whereas hands, feet, and areas with white hair respond poorly. Compared to long-standing patches, new ones are more likely to respond to medical therapy.
While the hair follicle is the main source of pigment restoration, another potential reservoir can be at the borders of the white patches. When successful re-pigmentation occurs, melanocyte stem cells (DOPA-negative) in the middle and lower outer root sheath (ORS), or bulge at the base of the hair follicle are activated (become larger, with intense DOPA oxidase activity). They migrate to the skin surface to form pigment islands, appearing as perifollicular brown macules. Otherwise, re-pigmentation can occur in less common patterns such as marginal, diffuse, or combined.
Treatment response is evaluated in terms of proportion of skin that has retained pigment. In studies, a good response is usually translated as > 50% or 75%, depending on the study’s design.
A cut, graze, or scratch may lead to a new patch of vitiligo
Cosmetic camouflage can disguise vitiligo. Options include:
Sun protection with clothing, sunscreen use, and lifestyle modification.
There are several modalities that are proven to be helpful in vitiligo. Optimal therapeutic response is often seen with combination therapies.
Calcineurin inhibitors (pimecrolimus cream and tacrolimus ointment)
Topical vitamin D derivatives (calcipotriol, tacalcitol)
Ruxolitinib cream
Other controversial therapies include pseudocatalase and topical prostaglandin inhibitors
Phototherapy refers to treatment with ultraviolet (UV) radiation. Options include:
Phototherapy probably works in vitiligo by two mechanisms.
Treatment is usually given twice weekly for a trial period of 3–4 months. If re-pigmentation is observed, treatment is continued until re-pigmentation is complete or for a maximum of 1–2 years.
A meta-analysis of 35 different studies reporting outcomes after phototherapy for generalised vitiligo. A marked or clinically useful response was achieved in 36% after 12 months of narrowband UVB and in 62% after 12 months of PUVA. The face and neck responded better than the trunk, which responded better than the extremities. It was not very effective on the hands and feet.
Oral minocycline 100 mg/day, a tetracycline antibiotic with anti-inflammatory properties
Subcutaneous afamelanotide
None of these treatments are based on randomised controlled trial data.
Surgical treatment for stable and segmental vitiligo requires removal of the top layer of vitiligo skin (by shaving, dermabrasion, sandpapering, or laser) and replacement with pigmented skin removed from another site.
Techniques include:
Depigmentation therapy, using 20% monobenzyl ether of hydroquinone (MBEH), may be considered in severely affected, dark-skinned individuals with vitiligo that has failed to re-pigment spontaneously or with therapy.
Cryotherapy and laser treatment (eg, 755-nm Q-switched alexandrite or 694 nm Q-switched ruby) have also been used successfully to depigment small areas of vitiligo.
Other novel potential therapies that are still under research include those targeting IFN-γ–JAK–STAT1 pathway (targeting CXCL9/10), anti-IL15 and anti-CD122 (targeting TRM), Wnt signalling antagonists, and others.
Vitiligo results in reduced quality of life and psychological difficulties in many patients, with problems like depression and poor self-esteem, especially in adolescents and in females. Patients should be assured that there is always something on the table to help in managing their condition, from using camouflage to available therapies with possible measurable improvement. The psychosocial impacts of vitiligo tend to be more severe in some countries, cultures, and religions than in others.
Family support, counselling, and cognitive behavioural treatment can be of benefit.
Unfortunately, there are no proven effective measures to prevent vitiligo. Although dogma related to many theories, ayurvedics, vitamin supplements, and alternative medicine has been endorsed by many vitiligo support groups, these are not based on scientific evidence. Aggressive treatment may help in halting the progression of a rapidly progressive disease.
The clinical course of generalised vitiligo is highly unpredictable.
In general, vitiligo progresses slowly and gradually over months, then remains quiescent for years, and is usually difficult to control.