Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Dr Achala Liyanage, Dermatology Fellow, Waikato Hospital, Hamilton, New Zealand; Assoc Prof Patrick Emanuel, Dermatopathologist, Auckland, New Zealand. January 2015.
Pityriasis lichenoides et varioliformis acuta (PLEVA) presents with haemorrhagic papules that resolve to leave varioliform scars. It is usually a self-limiting acute dermatosis. It is also known as Mucha Habermann disease.
PLEVA has sharply delimited, moderately dense, lymphocytic infiltrate involving the superficial vascular plexus, which extends in a wedge-shaped pattern to involve the lower dermis (figure 1). The superficial dermis shows a dense lichenoid infiltrate and impressive exocytosis of lymphocytes into the epidermis. The overlying stratum corneum shows parakeratosis which may be confluent and contain collections of neutrophils (figure 2). The epidermis shows pronounced hydropic change and foci of keratinocyte necrosis. Scattered extravasated erythrocytes are seen (figure 3).
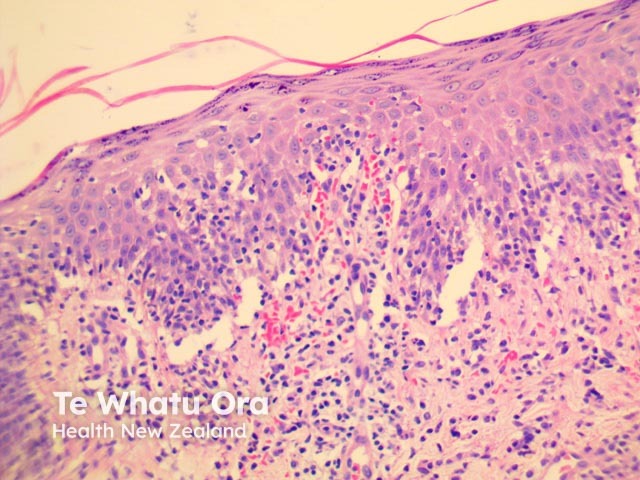
Figure 1
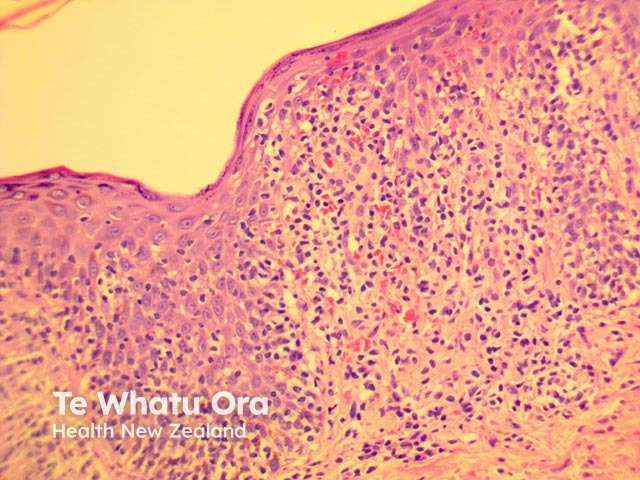
Figure 2
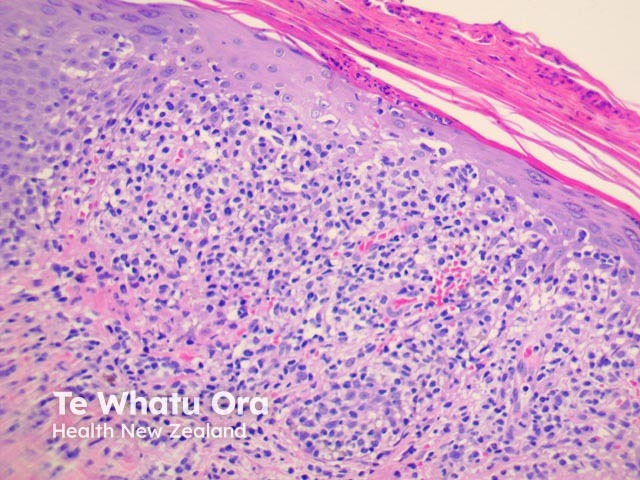
Figure 3

Figure 4
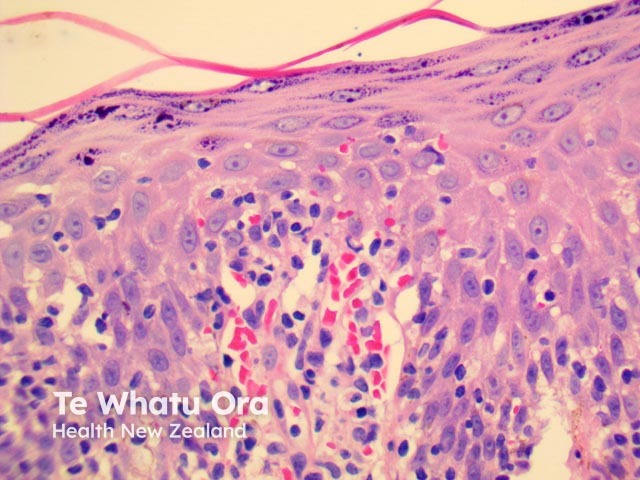
Figure 5
Images provided by Dr Duncan Lamont, Waikato Hospital
None are generally needed. Immunoperoxidase studies have shown the lymphocytic infiltrate consists of CD8/cytotoxic T cells.
Cutaneous T-cell lymphoma
Lymphocytic vasculitis