Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Dr Jacqueline Chen, General Practitioner, Australia (2022); Prof Amanda Oakley, Dermatologist, New Zealand (2015); minor update by Dr Jing Liu, Resident Medical Officer, Australia (2023)
Reviewing dermatologist: Dr Ian Coulson (2023)
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Lichen planus (LP) is a chronic inflammatory condition affecting the skin and mucosal surfaces. There are several clinical types:
Click here for images of lichen planus
Lichen planus affects approximately 1% of the population worldwide, mostly affecting adults aged between 30 to 60 years. It has no strong racial predilection.
Approximately 10% of those affected have lichen planus of the nails while half of those affected have oral lichen planus, which is more common in women than in men.
Lichen planus is a T-cell mediated autoimmune disorder in which inflammatory cells attack an unknown protein within the skin and basal keratinocytes.
Contributing factors to lichen planus may include:
Lichenoid inflammation is also notable in graft-versus-host disease.
Vitamin D deficiency may be associated with oral lichen planus. Its association with other types of LP remains unexplored.
Lichen planus may cause a small number or many lesions on the skin and mucosal surfaces.
The usual presentation of the disease is classical lichen planus. Symptoms can range from none (uncommon) to intense itch.

Papular lichen planus coalescing into plaques on the wrist (PLP-patient1)

Flat topped, shiny, polygonal papules of lichen planus on the volar wrist (PLP-patient1)

A plaque of lichen planus showing Wickham striae

Papular lichen planus with Koebner phenomenum in skin of colour

Lichen planus over the ankle and heel

Papular lichen planus with a linear Koebner lesion due to a scratch
Click here for more images of cutaneous lichen planus
The mouth is often the only affected area and often involves the inside of the cheeks and the sides of the tongue, but the gums and lips may also be involved.
The most common patterns are:
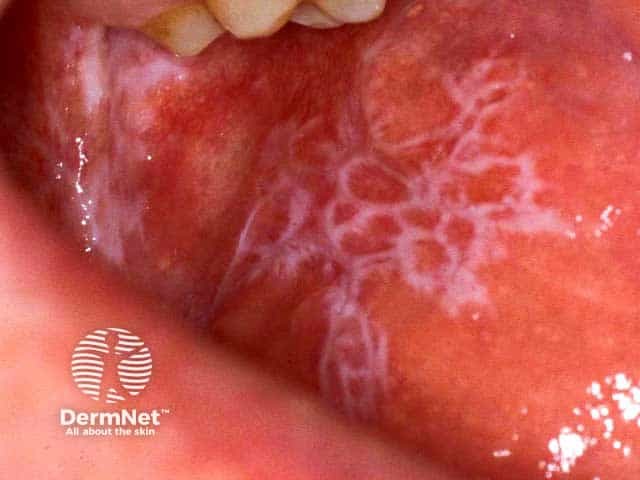
Reticulate buccal mucosal lichen planus

Lacy reticulated lichen planus covering the entire tongue

Erosive lichen planus on the lateral border of the tongue

Reticulate and violaceous lichen planus on the lower lip

Reticulate and eroded lichen planus on the lower lip
Click here for more images of oral lichen planus
Lichen planus may affect the labia majora, labia minora, and vaginal introitus. Presentation includes:
Click here for images of erosive vulval lichen planus
Click here for images of genital lichen planus
Erosive lichen planus uncommonly affects the lacrimal glands, eyelids, external ear canal, oesophagus, larynx, bladder, and anus.
Lichen planopilaris presents as tiny red spiny follicular papules and extending smooth areas on the scalp or less often, elsewhere on the body. Rarely, blistering occurs in the lesions. Destruction of the hair follicles leads to permanently bald patches characterised by sparse 'lonely hairs'.
Frontal fibrosing alopecia is a form of lichen planopilaris that affects the anterior scalp, forehead, and eyebrows.
Pseudopelade of Brocq may be a variant of lichen planus without inflammation or scaling. Areas of scarring without hair slowly appear, described as looking 'like footprints in the snow'.

Lichen planopilaris

Complete nail plate destruction due to lichen planus

Ridging and roughness (onychorrhexis) of the finger nail plates due to nail unit lichen planus

Nail plate atrophy and destruction and pterygium development in nail unit lichen planus. Lichen planus is evident over the adjacent distal phalanx
Click here for more images of nail lichen planus

Lichen planus pigmentosus of face

Lichen planus pigmentosus of lower back

Lichen planus pigmentosus of lower lip
Quinine and thiazide diuretics cause a photosensitive lichenoid drug eruption.
Bullous lichen planus
Lichen planus pemphigoides

Severe lichen planus on the foot producing blisters (BLP-patient1)
Hypertrophic, actinic variants, lichen planus pigmentosus, and residual post-inflammatory hyperpigmentation are more common amongst darker-skinned individuals.
Lichen planus is diagnosed clinically in most cases. A skin biopsy is often recommended to confirm the diagnosis and to look for cancer. The histopathological signs are of a lichenoid tissue reaction affecting the epidermis.
Typical features include:
Direct immunofluorescence studies are not routinely needed. Results may reveal colloid bodies in the papillary dermis with irregular deposits.
Patch testing may be recommended for patients with oral lichen planus affecting the gums and who have amalgam fillings, to assess for contact allergy to thiomersal (a mercurial compound) and other metals.
Differential diagnoses of lichen planus are broad and can be categorised into:
Papular classic |
|
Annular LP |
|
Linear |
|
Hypertrophic |
|
Lichen planus pigmentosus |
|
Lichen planus actinicus |
|
Vesicobullous |
|
Atrophic |
|
Vulval lichen planus |
|
Oral lichen planus |
|
Lichen planus of nails |
|
Lichen planopilaris |
Treatment is not always necessary as cutaneous LP can be self-limiting and treatment goals are to manage pruritus. Local treatments for the symptomatic cutaneous or mucosal disease are:
Systemic treatment for widespread lichen planus or severe local disease often includes a 1- to 3-month course of systemic steroids (eg, prednisone), while commencing another agent from the following list:
Anecdotal success is reported from long courses of antibiotics e.g. metronidazole, sulfasalazine, antifungals (such as griseofulvin), and JAK inhibitors. Lichen planopilaris is reported to improve with pioglitazone and tetracyclines.
In lichen planus actinicus, phototherapy should be avoided because lesions are typically triggered by sun exposure. Sun protection, including use of sunscreen, is an essential component of treatment.
In oral lichen planus, limited evidence is found in using apremilast. Successful treatment of oral and cutaneous lichen planus with adalimumab has previously been reported. Tildrakizumab has been shown to demonstrate positive results in erosive oral lichen planus in an isolated case study.
In cases of oral lichen planus affecting the gums and buccal mucosa with contact allergy to mercury, the lichen planus may resolve on replacing the fillings with composite material. If the lichen planus is not due to mercury allergy, removing amalgam fillings is very unlikely to result in a cure.
For more information see, oral lichen planus and erosive lichen planus.
Lichen planus can have a chronic remitting and relapsing course. Cutaneous lichen planus tends to clear within a couple of years in most people, but post-inflammatory pigmentation may take years to subside.
Mucosal lichen planus is more likely to persist for a decade or longer. For lichen planopilaris, scarring is permanent, including scarring alopecia. Lichenoid drug eruption resolves slowly when the responsible medication is withdrawn.