Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Kim Gear, Oral Medicine Trainee, Auckland, New Zealand, 2007. Updated by A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. January 2018. Minor amendment by Ian Coulson. July 2024.
Introduction
Demographics
Causes
Clinical features
Diagnosis
Complications
Management
Outcome
Oral lichen planus is lichen planus inside the mouth. Lichen planus is a chronic inflammatory skin condition.

Reticular lichen planus

Erosive lichen planus

Plaque lichen planus
Lichen planus affects about 1–2% of the adult population. It usually affects adults older than 45 years, with an average age at diagnosis of 50–60 years, although it may affect younger adults and children. It is more common in women than in men (1.4: 1). A history of lichen planus in family members is sometimes present.
Oral lichen planus affects 50% of patients with cutaneous lichen planus but may occur without skin lesions elsewhere.
The precise cause of oral lichen planus is not fully understood. It involves cytotoxic CD8+ T lymphocytes and pro-inflammatory cytokines, which attack the oral epithelial cells — resulting in their death. The immune response is mediated by antigen-specific cells.
In most cases oral lichen planus is idiopathic, when the reaction is thought to be against autoantigens. In other cases, it may be precipitated by exogenous antigens described below.
Oral lichenoid lesions are also part of the spectrum of chronic graft-versus-host disease that occurs after bone marrow transplantation.
Studies have demonstrated a lower serum vitamin D level in those with oral lichen planus compared to control groups.
Lichenoid drug reaction

Lichenoid reaction to amalgam

Graft versus host disease
Oral lichen planus can affect any or all areas inside the mouth. It can be precipitated by psychosocial stress or by local mechanical trauma.
Oral lichen planus may present in the following forms, and is often of mixed types.
Reticular lichen planus
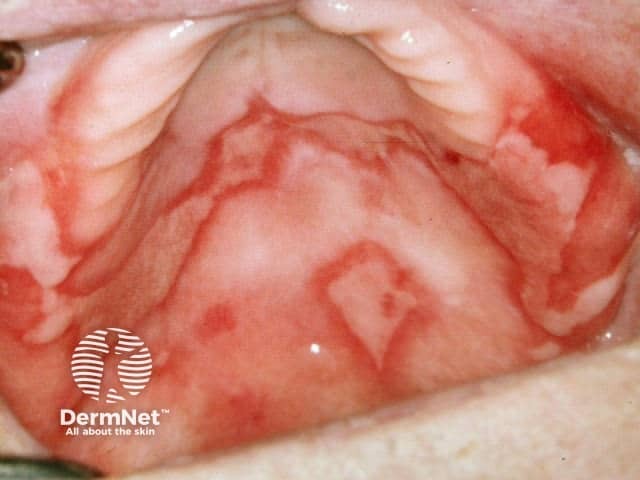
Atrophic/erosive lichen planus
Plaque type oral lichen planus

Reticular pattern

Erosive pattern

Plaque pattern
The diagnosis of oral lichen planus is often made by its clinical appearance. Tissue biopsy may be helpful, when characteristic features of lichen planus may be observed. Biopsy can help exclude other oral conditions with lichenoid reaction, such as drug-induced lichenoid reaction, oral lupus erythematosus, or a contact lichenoid reaction.
Under the microscope, the pathologist may observe a characteristic lichenoid reaction. Direct immunofluorescence may reveal positive staining for fibrinogen, immunoglobulins and complement.
Biopsy is often performed to rule out oral cancer.
Oral lichen planus can be very painful and ulceration may lead to scarring. Sometimes eating is so uncomfortable that the affected person is unable to maintain adequate nutrition.
Lichen planus, particularly the erosive form, may rarely lead to oral cancer (squamous cell carcinoma). Persistent ulcers and enlarging nodules should undergo biopsy.

Alveolar cancer
It is important to identify and remove or avoid any potential agent that might have caused a lichenoid reaction, such as drugs that have been started in recent months and contact allergens identified by patch testing.
Most people get satisfactory control of symptoms with the following measures.
In severe cases systemic corticosteroids may be used.
Other possible therapeutic agents may include:
Targeted molecular medicines are under investigation for the treatment or recalcitrant disease, with apremilast reported effective in a few patients.
The prognosis for oral lichen planus is uncertain. It can clear up within a few months or persist (with or without treatment) for decades. There are often periods of remission and relapse.