DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Fungal skin infections Tinea capitis CME
Fungal skin infections
Tinea capitis
Created 2009.
Learning objectives
- Identify and manage tinea capitis
Introduction
Tinea capitis most often presents in young children. In New Zealand, the zoophilic dermatophyte Microsporum canis has traditionally been the cause of tinea capitis and is due to contact with an infected kitten or rarely an older cat or dog. However in the last decade, T. tonsurans and T. violaceum have also become common causes of tinea capitis; these are anthropophilic organisms, i.e. they naturally infect humans. Anthropophilic tinea capitis may result in asymptomatic carriage in adults and children and can be transmitted by sharing hairbrushes and clothing.
Tinea capitis is classified according to how the fungus invades the hair shaft.
- Ectothrix infection (M. canis): hyphae and arthroconidia cover the outside of the hair. Ectothrix infections fluoresce green on Wood's light examination.
- Endothrix infection (T. tonsurans, T. violaceum): The hair shaft is filled with hyphae and arthroconidia. Endothrix infections do not fluoresce with Wood's light.
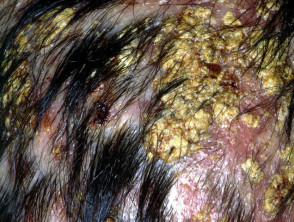
Tinea capitis may present in several ways.
- Dry scaling – like dandruff but usually with moth-eaten hair loss
- Black dots – the hairs are broken off at the scalp surface, which is scaly
- Smooth areas of hair loss (uncommon)
- Kerion – very inflamed abscess-like mass that may result in permanent scarring
- Carrier state – no symptoms and only mild scaling
Tinea capitis
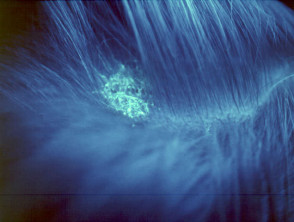
Wood's light examination
A Wood's light is a hand-held fluorescent lamp emitting "long wave" ultraviolet A. In dark conditions, certain infections fluoresce on exposure to the light.
- Fungal infection of the hair and scalp due to the cat ringworm Microsporum canis fluoresces green.
- Pityriasis versicolor, which mainly affects the trunk, is due to certain species of malassezia. It fluoresces yellow-green when the infection is active, providing the patient has not washed prior to examination (the responsible chemical is water soluble).
- Bacterial infection in skin flexures due to erythrasma Corynebacterium minutissimum fluoresces coral-pink.
As colour contrast increases on exposure to a Wood's light, the extent of pigmentary disorders can be determined.
- Vitiligo (white patches anywhere)
- Pityriasis versicolor (pale patches mainly on the trunk)
- Melasma (brown patches on the face)
Characteristic urinary fluorescence is also helpful in the diagnosis of hepatic porphyrias (porphyria cutanea tarda).
Wood's light
Management
First confirm the diagnosis of tinea capitis; use a toothbrush to obtain scrapings of scale and pluck a few loose hairs for mycology. Look for other sites of infection (feet, nails). Consider other reasons for scalp scaling and hair loss especially:
- Pityriasis capitis and seborrhoeic dermatitis (hair loss is uncommon, and if present tends to be diffuse). Microscopy may be positive for malassezia yeasts.
- Psoriasis (red scaly plaques, minimal hair loss, minimal symptoms, often signs elsewhere such as scalp, elbows, knees, flexures, nails)
- Alopecia areata (no scaling)
Tinea capitis requires oral antifungal treatment because topical agents are unable to penetrate to the base of the hair shaft. To reduce infectivity, it may be useful to wash the scalp using ketoconazole shampoo and to apply antifungal cream.
Oral therapy is required for four to eight weeks, usually terbinafine or itraconazole. Oral azoles require specialist approval for PHARMAC subsidy. Griseofulvin may be more effective for M. canis infections but is no longer readily available in New Zealand.
Treatment should be continued until scaling has cleared up and there is new healthy hair appearing. If in doubt, repeat mycology and continue to observe.
Activity
Immigrants from the African continent are particularly likely to be carriers of anthropophilic scalp fungi. Find out which measures have been proven to reduce transmission.
Related information
References:
On DermNet NZ:
Information for patients
Other websites:
- Medscape Reference: Tinea capitis
- Merck Manual Professional: Dermatophytoses
- Medscape:
Books about skin diseases:
See the DermNet NZ bookstore
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.