What is tuberous sclerosis?
Tuberous sclerosis or tuberous sclerosis complex (TSC) is a genetic disorder that is characterised by hamartomas in many organs, but particularly the skin, brain, eye, kidney and heart. Hamartomas are non-cancerous malformations composed of an overgrowth of the cells and tissues that normally occur in the affected area and include naevi (birthmarks). Tuberous sclerosis is also known as epiloia.
Skin lesions, epileptic seizures and developmental delay/behavioural problems are the main features of tuberous sclerosis complex. However, individuals with the condition may be affected in many different ways and with differing degrees of severity. Some patients may have very few, or no symptoms at all, while others may be severely affected with a multitude of symptoms.
What causes tuberous sclerosis and who gets it?
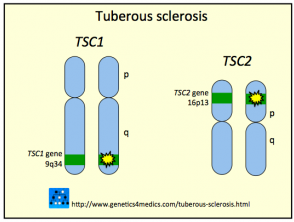
Tuberous sclerosis is a genetic disorder due to a mutation in one of two genes:
- TSC1, which produces a protein called hamartin (10–30% of cases)
- TSC2, which produces a protein called tuberin
About one-third of all cases of tuberous sclerosis are inherited from an affected parent. All other cases are due to sporadic new mutations occurring in the early stages of life, most often mutations of TSC2.
People of all races and sex may be affected. The condition may become apparent any time from infancy to adulthood but usually occurs between 2-6 years of age.
Genetics of Tuberous sclerosis*
*Image courtesy Genetics 4 Medics
What are the skin signs of tuberous sclerosis complex?
Skin lesions are found in 60-70% of cases of tuberous sclerosis.
| Lesion | Features |
|---|---|
| Angiofibromas |
|
Angiofibromas |
|
| Ungual fibromas |
|
Periungual fibromas |
|
| Shagreen patch |
|
Shagreen patches |
|
| Ovoid or ash leaf-shaped white macules |
|
Ash leaf marks |
|
See more images of tuberous sclerosis.
Other organ involvement
Epilepsy is present in about 70% of patients with tuberous sclerosis.
- Usually begins in infancy or early childhood and may precede the appearance of skin lesions by years
- The greater the number of tumours (cortical tubers) in the brain, the greater the severity of seizures.
Developmental delay and behavioural problems may also occur. Symptoms include mild to severe intellectual disability, autism, attention deficit disorder (ADD), anxiety, depression, paranoia and schizophrenia.
Other signs and symptoms of tuberous sclerosis include:
- Eye involvement: white spots on the iris and white lumps on the retina
- Heart, gastrointestinal and kidney tumours
- Lung changes
What treatment is available?
Tuberous sclerosis is a multisystem disorder, so treatment from a team of specialist doctors is usually necessary.
Skin lesions, particularly facial angiofibromas, may be psychologically distressing for some patients. Laser treatment or electrosurgery can be used to remove angiofibromas.
The topical mTOR inhibitor sirolimus 0.2% gel (also called rapamycin) has proved helpful in reducing angiofibromas in a clinical trial involving 36 adults and children. One study has also reported improvement in hypopigmented macules. A larger prospective, multicentre, randomised, double-blind, vehicle-controlled trial enrolled 179 patients with tuberous sclerosis-related facial angiofibromas and found improvement in more than 80% of patients treated with topical 1% rapamycin with most occurring in the first month. It was well tolerated [5–8].