Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Dr Alice Manley, Core Medical Trainee, Southmead Hospital, North Bristol Trust, United Kingdom. DermNet Editor in Chief: A/Prof. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. February 2019.
Introduction Demographics Causes Clinical features Complications Diagnosis Treatment Outcome
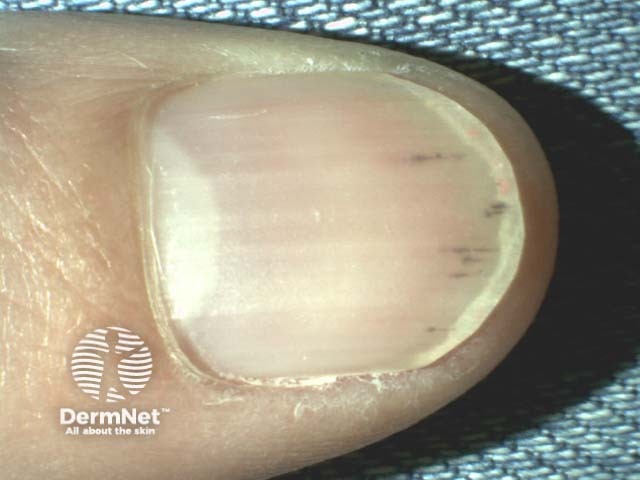
A splinter haemorrhage is a longitudinal, red-brown haemorrhage under a nail and looks like a wood splinter. Seen end-on, the haemorrhage is in the lower part of the nail plate or underneath it.
Splinter haemorrhages

Splinter haemorrhages

Splinter haemorrhages seen end on
Splinter haemorrhages can occur at any age; however, they are more common in older people [1,2].
The most common cause of a splinter haemorrhage is trauma, including the application of an acrylic nail [3]. The longitudinal nature of splinter haemorrhages is explained by the orientation of the capillaries in the nail bed.
Splinter haemorrhages are present in 15–33% of patients with infective endocarditis in association with Osler nodes and Janeway lesions [3]. They may be due to septic emboli in the small vessels of the nail bed and the increased fragility of the vessel walls in sepsis [2,3].
Other infective causes include:
Splinter haemorrhages are common signs of psoriatic nail disease and nail disease due to lichen planus [3]. They can also be associated with a tumour.

Psoriasis

Psoriasis

Onychopapilloma
Splinter haemorrhages may be due to microemboli or injury to vessel walls associated with vasculitis, including systemic diseases such as [3]:
Splinter haemorrhages are observed in patients with chronic kidney disease on haemodialysis or post-renal transplant, and may be explained by abnormal coagulation [3].
Medications associated with splinter haemorrhages include [3]:
Splinter haemorrhages present as longitudinal 1–3 mm red lines under the nail plate [2,3].
There are no complications of splinter haemorrhages themselves; complications arise as a consequence of the underlying disease process.
A careful history and physical examination are required to determine the underlying cause.
The diagnosis of splinter haemorrhages is made clinically or with the aid of dermatoscopy [1].

Splinter haemorrhage dermoscopy

Splinter haemorrhage dermoscopy

Splinter haemorrhage dermoscopy
There is no specific treatment for a splinter haemorrhage.
Any treatment is targeted at an underlying systemic condition or at discontinuing a causative drug.
If caused by trauma, a splinter haemorrhage grows out and disappears. Haemorrhages may continue to recur if the underlying cause remains.