Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Dr Chelsea Jones, Newcastle, Australia; Dr Monisha Gupta, Dermatologist, Australia (2020); updated by Dr Salim Uddin, Medical Registrar, New Zealand; A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand (2023). Minor update November 2025.
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Classification
Types
Variation in skin types
Aggravating factors
Diagnosis
Treatment
E-lecture
Psoriasis is a chronic inflammatory skin condition characterised by clearly defined, red and scaly plaques. It is classified into several types.
Psoriasis affects 2–4% of males and females. It can start at any age including childhood, with onset peaks at 15–25 years and 50–60 years. It tends to persist lifelong, fluctuating in extent and severity. It is particularly common in Caucasians but may affect people of any ethnicity. About one-third of patients with psoriasis have family members with psoriasis.
Psoriasis is multifactorial. It is classified as an immune-mediated genetic skin disease.
This involves a complex interaction between the innate and adaptive immune systems.
Genome-wide association studies report that the histocompatibility complex HLA-C*06:02 (previously known as HLA-Cw6) is associated with early-onset psoriasis and guttate psoriasis. This major histocompatibility complex is not associated with psoriatic arthritis, nail psoriasis, or late-onset psoriasis.
Immune factors and inflammatory cytokines (messenger proteins) such as IL1β and TNFα, IL-23, and IL-17 are responsible for the clinical features of psoriasis. These have therefore become targets for biological drugs and have led to success in drug management.
Psoriasis usually presents with symmetrically distributed, red, scaly plaques with well-defined edges. The scale is typically silvery white, except in skin folds where the plaques often appear shiny with a moist peeling surface. The most common sites are the scalp, elbows, and knees, but any part of the skin can be involved. The plaques are usually very persistent without treatment.
Itch is mostly mild but may be severe in some patients, leading to scratching and lichenification characterised by thickened leathery skin and increased skin markings. Painful skin cracks or fissures may occur, particularly on the palms and soles.
Psoriasis can demonstrate the Koebner phenomenon. This involves the generation of new lesions on the skin that has been damaged or irritated such as by injury, burns etc.
When psoriatic plaques clear up, they may leave brown or pale marks (postinflammatory hypo- or hyperpigmentation) that can be expected to fade over several months.
Auspitz sign refers to pinpoint bleeding upon removal of the scaly layer in plaque psoriasis. It is related to the dilated dermal capillaries involved in the histological pathogenesis of chronic psoriasis.
Certain features of psoriasis can be categorised to help determine appropriate investigations and treatment pathways - overlap may occur. These include:
Post-streptococcal acute guttate psoriasis

Small plaques of psoriasis appear almost like rain drops splashed over the skin

Close up of guttate psoriasis

Post-inflammatory hypopigmentation as guttate psoriasis is resolving

Well demarcated plaques with silvery scale in chronic plaque psoriasis

Thick silvery scale over the elbow

Close up of well demarcated plaques with silvery scale in chronic plaque psoriasis

Well demarcated salmon pink erythema which extends to the apex of the skin fold due to flexural psoriasis

Well demarcated salmon pink erythema which extends to the apex of the skin fold and into the natal cleft due to flexural psoriasis

Axillary psoriasis

Well demarcated plaques of scalp psoriasis

Scalp psoriasis often extends beyond the hair line
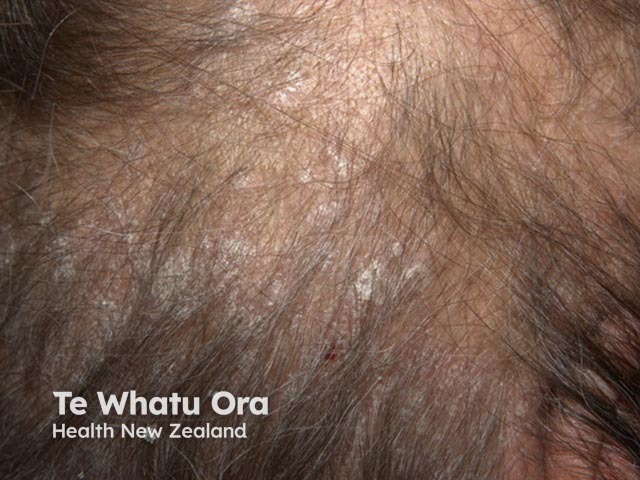
Adherent scale in scalp psoriasis

Sebopsoriasis of ear

Sebopsoriasis of chest

Sebopsoriasis affecting the retroauricular skin

Hyperkeratosis of the soles and heels due to psoriasis - painful fissuring is often a problem

Palmar plaque psoriasis

Hyperkeratosis of the soles and heels due to psoriasis

Irregular pits and onycholysis of a finger nail - note the yellow band proximal to the onycholysis

Onycholysis, proximal yellow band and nail plate splitting due to nail unit psoriasis

Onycholiasis (separation of the plate from the bed) due to psoriasis

Confluent skin redness and scaling - the patient was shivery and feels unwell

Confluent redness affecting more than 80% of the body – erythrodermic psoriasis

Close up of the confluent redness and scale in erythrodermic psoriasis
There is some controversy as to whether generalised pustulosis and localised palmoplantar pustulosis are classified as being within the psoriasis spectrum.
Plaque psoriasis is the most common type of psoriasis in all racial groups. Non-Caucasians tend to have more extensive skin involvement than Caucasians. Asian populations are reported to have the highest percentage of body surface area involvement.
In skin of colour, the plaques are typically thicker with a more pronounced silver scale and itch. The pinkness of early patches may be more difficult to appreciate.
Thick plaques may appear violet or dark in colour. Plaque psoriasis is more likely to result in postinflammatory hyperpigmentation or hypopigmentation in the skin of colour, which further impacts the quality of life even after disease clearance.
Other types of psoriasis show variable rates in different skin types. Palmoplantar psoriasis is reported to be more common in the Indian population. Non-Caucasians are more likely to present with pustular and erythrodermic psoriasis than Caucasians, whereas flexural psoriasis is said to occur at a lower rate in skin of colour.

Chronic plaque psoriasis in skin of colour

Chronic plaque psoriasis in skin of colour

Small plaque psoriasis with prominent scale in skin of colour
Patients with psoriasis are more likely than others to have associated health conditions such as are listed here.
Metabolic syndrome refers to the combination of obesity, hypertension, dyslipidaemia, and insulin resistance.
Lifestyle modifications such as weight loss, lipid profile reduction, and tight control of glucose levels reduce the mortality from cardiovascular events in patients with psoriasis.
Psoriasis is diagnosed by its clinical features. If necessary, diagnosis is supported by typical skin biopsy findings.
Medical assessment entails a careful history, examination, questioning about the effect of psoriasis on daily life, and evaluation of comorbid factors.
Validated tools used to evaluate psoriasis include:
The severity of psoriasis is classified as mild in 60% of patients, moderate in 30% and severe in 10%.
Evaluation of comorbidities may include:
Patients with psoriasis should be well-informed about their skin condition and its treatment. Recommendations include:
Mild psoriasis is generally treated with topical agents alone. The selected treatment depends on the body site and the extent and severity of psoriasis, and may include:
Most psoriasis centres offer phototherapy (light therapy) with ultraviolet (UV) radiation, often in combination with topical or systemic agents, including:
Moderate to severe psoriasis warrants treatment with a systemic agent and/or phototherapy. The most common treatments are:
Other medicines occasionally used for psoriasis include:
Systemic corticosteroids are best avoided due to the risk of severe withdrawal flare of psoriasis and adverse effects.
Biologic or biological therapy is reserved for severe psoriasis and psoriatic arthritis that have failed to respond to conventional systemic therapy. The use of biologics has increased with the development of novel therapies targeting key inflammatory pathways such as TNF-alpha and IL-17.
Biologics are costly and may result in side effects. They should be initiated by specialists familiar with their use.
Interleukin 17 (IL-17) inhibitors:
Interleukin 23 (IL-23) inhibitors:
Adalimumab, etanercept, and ustekinumab have been used to treat severe psoriasis in children.
Newer agents: