Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Elizabeth Brown, Medical Student, Waikato Clinical School, Auckland University Faculty of Medical and Health Sciences, 2013.
Introduction
Types
Causes
Diagnosis
Severity assessment
Treatment
Outlook
Psoriasis is a chronic skin condition that occurs in children and adults. The typical appearance is of red, thickened, scaly patches on the skin (plaques). These plaques can vary in size and distribution from person to person. In some people, it may affect small areas of skin while others may have large areas covering their body.

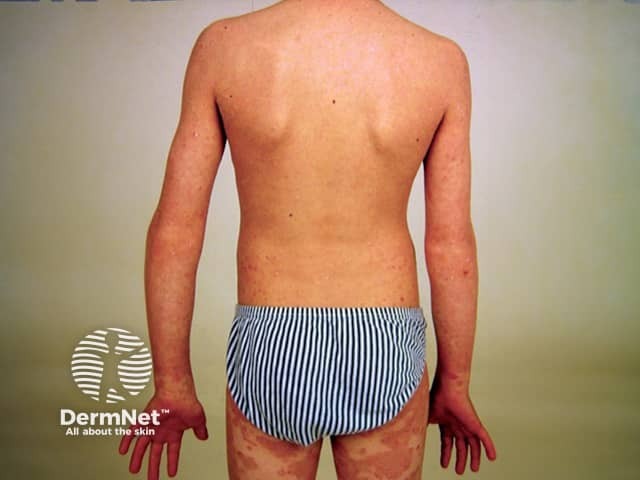
Guttate psoriasis in child

Psoriasis in child

Psoriasis in child

Facial psoriasis in child

Scalp psoriasis in child
Erythrodermic psoriasis in child
Each of the patterns of psoriasis described in adults can be seen in children. These include:
Guttate, facial and flexural psoriasis are particularly common in children.
Psoriasis has a strong genetic component and is due to abnormal processes involved in the regulation of the immune system.
Individuals may have flares of psoriasis in response to stress, injury, medications and infections (particularly streptococcal tonsillitis).
Psoriasis is not contagious, therefore, affected children do not need to be isolated from other children.
The diagnosis of psoriasis is usually made clinically. This involves a doctor examining the skin and making the diagnosis based on the appearance of the affected areas.
Occasionally, a skin biopsy may be necessary to distinguish psoriasis from other skin conditions that may appear similar.
Assessing the severity of psoriasis can assist in deciding upon the most appropriate course of treatment. The severity of psoriasis can be determined in the following ways:
Individuals with severe psoriasis are best managed by a specialist dermatologist. Children and adolescents with psoriasis can experience significant psychological and social effects and may require input from a paediatric dermatologist, paediatrician and counsellors.
Although there is no cure, several treatment options are available to manage psoriasis.
Topical therapies are suitable for all children with psoriasis and may be all that is required for mild to moderate psoriasis.
Narrowband UVB phototherapy is often used in children with psoriasis, especially in those over 10 years of age. Thin chronic plaque psoriasis and guttate psoriasis respond best. A hospital-based course of treatment usually requires attendance 3 times weekly for 6 to 12 weeks. Broadband UVB and PUVA are available in some centres.
Methotrexate tablets prescribed off-label once weekly are useful in children that have not improved satisfactorily with topical preparations or phototherapy. The data on the use of methotrexate is less extensive in children compared to adults. However, several case reports have shown significant clinical improvement in children as young as 2 years old, with excellent tolerance. Regular blood tests are required to monitor safety.
Biologic agents (e.g. subcutaneous etanercept and intravenous infliximab injections) should only be used in children with severe psoriasis that does not respond to other therapies. Biologics are considered to be safe in children although serious adverse effects (especially infection) have been reported. Use of a biological agent will be made in consultation with a dermatologist on a case by case basis.
Psoriasis in children may completely clear up within months of presentation, especially if guttate plaques occur in response to an infection. However, some children progress to have long-term psoriasis, often life-long. Early-onset large chronic plaque psoriasis tends to be particularly persistent and challenging to treat. Complications such as psoriatic arthritis and non-alcoholic fatty liver disease may occur.
Children with severe psoriasis should be advised to maintain a healthy weight, take regular exercise, and to avoid smoking.