Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Reactions Infections Treatments
Author: Dr Aarthy Uthayakumar, Core Medical Trainee, University College Hospital London, London, United Kingdom. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. March 2018.
Introduction Introduction - adverse drug reaction Demographics Classification Classification of cutaneous drug reactions Differential diagnoses Classification Diagnosis Treatment Conclusion
Antibiotics are drugs used to treat bacterial infections.
An adverse drug reaction (ADR) is an unintended response to a drug at doses normally used for disease therapy. Cutaneous ADRs are ADRs affecting the skin.

Morbilliform eruption

Acute urticaria

Fixed drug eruption
Adverse drug reactions are common, particularly in hospital inpatients, with estimates of 2–3% of hospitalised patients experiencing an ADR, and one in 20 of them being potentially fatal.
Cutaneous ADRs account for 10–30% of ADRs, and are most commonly due to antibiotics. The reactions can vary in severity; most are mild-to-moderate, but severe reactions are estimated to occur in 0.1–2% of cases.
Adverse drug reactions can be classified as either non-immunological or immunological.
Non-immunological ADRs caused by antibiotics include:

Oral candidiasis

Gram negative folliculitis

Malassezia folliculitis
There are four main types of immunologically mediated hypersensitivity or allergic responses to drugs. These immunological ADRs make up approximately 20% of ADRs.
Severe ADRs to some antibiotics, such as Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) due to sulphonamides, are caused by complex immunological mechanisms.
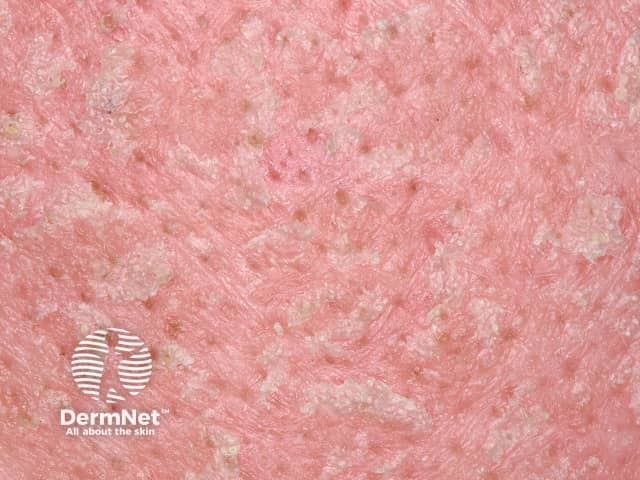
Rashes due to antibiotics are most often morbilliform (exanthematous) or urticarial.
It usually takes 7–10 days to become allergic to a drug, so if a reaction is rapid, it is either non-immunological, or it is due to a previous encounter with the same drug or a chemically similar substance.

Morbilliform rash

Urticaria

Urticaria
Several other ADRs affecting the skin can be due to antibiotics and are listed below alphabetically.

Acute generalised exanthematous pustulosis

Angioedema
Drug hypersensitivity syndrome

Oral pemphigus

Erythema multiforme

Hypersensitivity vasculitis

Photosensitivity

Toxic epidermal necrolysis

SDRIFE
It is sometimes difficult to determine whether an antibiotic has caused a rash. Drugs are rarely deliberately given to the affected patient again, as re-challenge has the potential to cause a life-threatening response in some cases. This means the true incidence of ADRs is difficult to calculate.
There are important differential diagnoses to consider when examining a suspected cutaneous drug reaction; these include:
A large number of antibiotics have the potential to cause cutaneous drug reactions.
The four classes of beta-lactam antibiotics are penicillins, cephalosporins, carbapenems, and monolactams. Allergic reactions to beta-lactam antibiotics are the most common cause of immunological ADRs. This is thought to be due to the structure of beta-lactams. IgG antibodies to penicillin can be detected in allergic patients and non-allergic patients taking penicillin.
There is some cross-reactivity between penicillins and cephalosporins. If a patient has an anaphylactic response to penicillins, cephalosporins should be avoided.
Cutaneous ADRs caused by beta-lactams include:
Though structurally similar, carbapenems can usually be safely used in patients with anaphylactoid reactions to penicillin. The major non-cutaneous side effects of beta-lactam use are diarrhoea, increased Clostridium (Clostridioides) difficile, and drug-induced liver injury, particularly due to clavulanic acid/amoxicillin.
In comparison to most other antibiotics, macrolides are considered relatively safe drugs.
Tetracycline antibiotics are frequently used in dermatology. Possible cutaneous reactions include:
Several older generation fluoroquinolones have been withdrawn from the market due to severe adverse reactions including photosensitivity.
Side effects of current-generation quinolones include tendinopathy and QT prolongation. Common cutaneous reactions include:
Co-trimoxazole is a sulfonamide antibiotic commonly used in immunocompromised individuals, who are already more at risk of ADRs. The most frequent ADRs are morbilliform or urticarial rash; however, serious ADRs can result, most commonly SJS/TEN. Observed cutaneous drug reactions with sulfonamides include:
Non-cutaneous reactions with sulfonamides include thrombocytopenia, anaemia, and electrolyte abnormalities.
It is essential to take a careful history in the diagnosis of cutaneous drug reactions. Many affected patients have been taking several drugs. In these cases, it helps to form a timeline, including the initiation of any new drugs and the rash onset.
Sometimes, a skin biopsy will be taken to clarify the inflammatory pattern. The presence of eosinophils can be a helpful clue of an underlying drug cause but is non-specific.
Skin testing is sometimes undertaken, especially for penicillin.
The first principle of management is the withdrawal of the causative drug.
Other measures include:
Antibiotics are one of the most significant discoveries in medicine, but they are not without complications.
Cutaneous side effects are commonly experienced and have the potential to be life-threatening, especially in at-risk groups. Among the classes, penicillins, cephalosporins, sulfonamides, and fluoroquinolones are the most common causes of cutaneous reactions, particularly severe ones.