Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Vanessa Ngan, Staff Writer; Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, 2003. Updated by Dr Delwyn Dyall-Smith, 2009. Further updated by Dr Amanda Oakley, January 2016.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outlook
Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are now believed to be variants of the same condition, distinct from erythema multiforme. SJS/TEN is a rare, acute, serious, and potentially fatal skin reaction in which there are sheet-like skin and mucosal loss. Using current definitions, it is nearly always caused by medications.
SJS/TEN is a very rare complication of medication use (estimated at 1–2/million each year for SJS, and 0.4–1.2/million each year for TEN).
Genetic factors are important.
More than 200 medications have been reported in association with SJS/TEN.
The drugs that most commonly cause SJS/TEN are antibiotics in 40%. Other drugs include:
SJS/TEN is a rare and unpredictable reaction to a medication. The mechanism has still not been understood and is complex.
Drug-specific CD8+ cytotoxic lymphocytes can be detected in the early blister fluid. They have some natural killer cell activity and can probably kill keratinocytes by direct contact. Cytokines implicated include perforin/granzyme, granulysin, Fas-L and tumour necrosis factor alpha (TNFα).
There are probably two major pathways involved:
SJS/TEN usually develops within the first week of antibiotic therapy but up to 2 months after starting an anticonvulsant. For most drugs, the onset is within a few days up to 1 month.
Before the rash appears, there is usually a prodromal illness of several days duration resembling an upper respiratory tract infection or 'flu-like illness. Symptoms may include:
There is then an abrupt onset of a tender/painful red skin rash starting on the trunk and extending rapidly over hours to days onto the face and limbs (but rarely affecting the scalp, palms or soles). The maximum extent is usually reached by four days.
The skin lesions may be:
The blisters then merge to form sheets of skin detachment, exposing red, oozing dermis. The Nikolsky sign is positive in areas of skin redness. This means that blisters and erosions appear when the skin is rubbed gently.

Toxic epidermal necrolysis

Toxic epidermal necrolysis

Toxic epidermal necrolysis
Mucosal involvement is prominent and severe, although not forming actual blisters. At least two mucosal surfaces are affected including:
The patient is very ill, extremely anxious and in considerable pain. In addition to skin/mucosal involvement, other organs may be affected including liver, kidneys, lungs, bone marrow and joints.

Toxic epidermal necrolysis

Stevens Johnson Syndrome

Stevens Johnson Syndrome
SJS/TEN can be fatal due to complications in the acute phase. The mortality rate is up to 10% for SJS and at least 30% for TEN.
During the acute phase, potentially fatal complications include:
SJS/TEN is suspected clinically and classified based on the skin surface area detached at maximum extent.
SJS
Overlap SJS/TEN
TEN with spots
TEN without spots
The category cannot always be defined with certainty on initial presentation. The diagnosis may, therefore, change during the first few days in the hospital.
If the test is available, elevated levels of serum granulysin taken in the first few days of a drug eruption may be predictive of SJS/TEN.
Skin biopsy is usually required to confirm the clinical diagnosis and to exclude staphylococcal scalded skin syndrome (SSSS) and other generalised rashes with blisters
The histopathology shows keratinocyte necrosis (death of individual skin cells), full thickness epidermal/epithelial necrosis (death of an entire layer of skin), minimal inflammation (very mild lymphocytic infiltrate of the superficial dermis). The direct immunofluorescence test on the skin biopsy is negative, indicating the disease is not due to deposition of antibodies in the skin.
Blood tests do not help to make the diagnosis but are essential to make sure fluid and vital nutrients have been replaced, to identify complications and to assess prognostic factors (see below). Abnormalities may include:
In vitro diagnostic tests for drug allergies including SJS/TEN are under investigation.
Patch testing rarely identifies the culprit in SJS/TEN, and is not recommended.
SCORTEN is an illness severity score that has been developed to predict mortality in SJS and TEN cases. One point is scored for each of the seven criteria present at the time of admission. The SCORTEN criteria are:
The risk of dying from SJS/TEN depends on the score.
In 2019, a new prediction model was proposed, the ABCD-10.
A: age over 50 years (one point)
B: bicarbonate level < 20 mmol/L (one point)
C: cancer present and active (two points)
D: dialysis prior to admission (3 points)
10: epidermal detachment ≥ 10% body surface area on admission (one point)
The ABCD-10 was evaluated in a cohort of 370 patients >with SJS/TEN in multiple institutions in the USA and predicted in-hospital mortality as well as SCORTEN. The predicted mortality rates in this cohort are shown in the table.
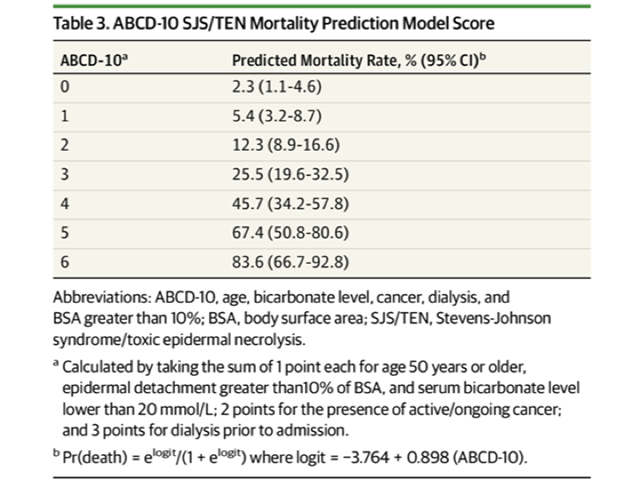
ABCD 10 Mortality prediction model score
Validation in other populations is required.
In the differential diagnosis of SJS/TEN consider:
For further details, see Stevens Johnson syndrome / toxic epidermal necrolysis: nursing management.
Care of a patient with SJS/TEN requires:
Skin care
Eye care
Mouth care
Genital care
Lung care
Urinary care
General
The role of systemic corticosteroids (cortisone) remains controversial. Some clinicians prescribe high doses of corticosteroids for a short time at the start of the reaction, usually prednisone 1–2 mg/kg/day for 3–5 days. However concerns have been raised that they may increase the risk of infection, impair wound healing and other complications, and they have not been proven to have any benefit. They are not effective later in the course of the illness.
Case reports and small patient series have reported benefit from active adjuvant treatments delivered during the first 24–48 hours of illness. As SJS/TEN is a rare condition, controlled trials of therapies in large numbers of patients are difficult.
Ciclosporin 3–5 mg/kg/day is reported to reduce mortality by 60% compared to patients with similar SCORTEN score on admission that were not treated with ciclosporin. There are contraindications to treatment such as renal impairment.
Other options include:
Thalidomide, trialled because of its anti-TNFα effect, increased mortality, and should not be used.
People who have survived SJS/TEN must be educated to avoid taking the causative drug or structurally related medicines as SJS/TEN may recur. Cross-reactions can occur between:
In the future, we may be able to predict who is at risk of SJS/TEN using genetic screening.
Allopurinol should be prescribed for good indications (eg, gout with hyperuricaemia) and commenced at a low dose (100 mg/day), as SJS/TEN is more likely at doses > 200 mg/day.
The acute phase of SJS/TEN lasts 8–12 days.
Repithelialisation of denuded areas takes several weeks and is accompanied by peeling of the less severely affected skin. Survivors of the acute phase have increased on-going mortality especially if aged or sick.
Long-term sequelae include:
Eye problems can lead to blindness:
It may take weeks to months for symptoms and signs to settle.

Dyspigmentation

Nail shedding

Symblepharon