Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Systemic diseases Autoimmune/autoinflammatory
Author: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, February 2015.
Introduction
Causes
Demographics
Cutaneous features
Systemic features
Diagnosis
Treatment
Outlook
Lupus erythematosus (LE) is a group of diverse, persistent autoimmune inflammatory diseases.
Systemic lupus erythematosus (SLE) affects several organs (such as skin, joints and kidneys) and blood tests reveal circulating autoantibodies. The clinical features of SLE are highly variable and may overlap with other diseases and conditions. Skin involvement or cutaneous lupus (CLE) affects 80% of patients with SLE.
SLE is sometimes called acute lupus erythematosus, and the cutaneous features may be described as acute cutaneous lupus.
Factors leading to SLE include:
The manifestations of SLE are due to loss of regulation of the patient's immune system.
SLE can affect males and females of any age. Every year about 2–7 new cases are diagnosed in a population of 100,000 people. SLE is much more common in females than males, and onset is most often between the ages of 15 and 45 years.
SLE is more prevalent and more severe in smokers. Smoking also reduces the effectiveness of antimalarials and other therapies.
Autoantibodies can be present in people that have no manifestation of the disease.
About 80% of patients with SLE have skin involvement (cutaneous LE), and it is the first sign of SLE in about one-quarter of them. It can present as LE-specific or LE-nonspecific manifestations. LE-specific lesions tend to be induced or aggravated by exposure to ultraviolet radiation and are localised in sun-exposed sites such as the face, neck, V of the neck and upper back.
Cutaneous lupus (CLE) has specific acute, subacute and chronic manifestations.

Butterfly rash

Bullous LE

Mucosal ulceration

Diffuse hair loss

Systemic lupus erythematosus

Systemic lupus erythematosus

Systemic lupus erythematosus
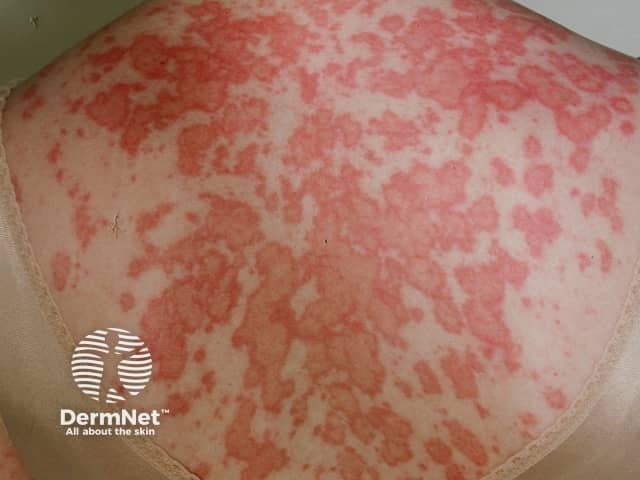
Systemic lupus erythematosus
See more images of cutaneous lupus erythematosus.

Tumid CLE

Lupus profundus

Mucosal CLE
Nonspecific cutaneous SLE refers to features relating to underlying illness rather than an autoimmune attack. These features may occur in other connective tissue and autoimmune diseases.

Nail-fold capillaries

Vasculopathy

Palpable purpura

Livedo reticularis
Numerous systemic features may occur in SLE and can result in critical illness.
SLE can be difficult to diagnose at times because of the great variety of presentations of the disease, and the presence of similar symptoms in people that do not have the disease. Several attempts have been made to help clinicians reach the diagnosis, including the American College of Rheumatology criteria for the classification of SLE (revised in 1997). In 2012, the criteria were revised by the Systemic Lupus International Collaborating Clinics (SLICC).[1]
Using the SLICC criteria, SLE is diagnosed if the patient has either of the following over time:
These criteria depend on history, clinical examination, exclusion of other causes of the symptoms, and the results of investigations—including blood tests and biopsy of the affected tissue. Four of the 17 SLICC criteria relate to the skin.
* SLICC Systemic Lupus International Collaborating Clinics; ANA antinuclear antibody; anti-dsDNA anti-double-stranded DNA
The Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) was developed in an attempt to classify the severity of CLE. [2] A score of activity and damage due to the disease is calculated in each of 12 anatomical locations (refer to the original published paper for details).
The total activity score is made up of:
Total damage score is made up of:
Patients with SLE often undergo skin biopsy.
Multiple autoantibodies are typically present in SLE, often in high titre (see immunological criteria above). Relating to skin disease in SLE:
Patients with SLE should also have renal, liver and thyroid function and markers of inflammation performed, such as C-reactive protein (CRP), immunoglobulins and rheumatoid factor.
Photoprovocation tests are sometimes carried out to confirm that a skin eruption is precipitated by exposure to particular wavelengths of ultraviolet or visible radiation.
Other tests depend on which organ is affected. They may, for example, include:
The following measures are essential to reduce the chance of flares and organ damage.
Intermittent courses of potent topical corticosteroids are important in the treatment of CLE. They should be applied accurately to the skin lesions.
The calcineurin inhibitors tacrolimus ointment and pimecrolimus cream can also be used.
Treatment of SLE depends on which are the predominant organs involved in the disease. Typically, any of the following drugs may be used alone or in combination.
CLE is also sometimes treated with:
SLE leads to a chronic illness with flares and periods of remissions. In some patients, all signs of active disease resolve in time.