Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Autoimmune/autoinflammatory Rashes
Author: Amanda Oakley, Dermatologist, Hamilton, New Zealand, 2001/2016
DermNet Update April 2021; further minor update September 2024.
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Treatment
Outcome
Cutaneous lupus erythematosus (LE) is a diverse group of autoimmune connective tissue disorders localised to the skin that can be associated with systemic lupus erythematosus (SLE) to varying degrees.
Cutaneous lupus erythematosus (CLE) is classified as:

Acute cutaneous LE

Subacute cutaneous LE

Chronic cutaneous LE
Skin lesions of cutaneous lupus erythematosus can be subdivided into:
Cutaneous lupus erythematosus has an annual incidence of 4 cases per 100,000 people, and a prevalence of 73 cases per 100,000.
As with SLE, there is a marked female predominance with CLE particularly affecting women 20 to 50 years of age. However, all age groups and both sexes can be affected. Skin of colour is an important predisposing factor.
Up to 75% of patients with SLE develop cutaneous signs, and these may be the first indication of SLE in 25%.
The pathogenesis of cutaneous lupus erythematosus is multifactorial:
This is a brief overview of the clinical features of cutaneous lupus erythematosus. See the specific lupus pages for more detail – links are provided at the end under the ‘On DermNet’ heading.
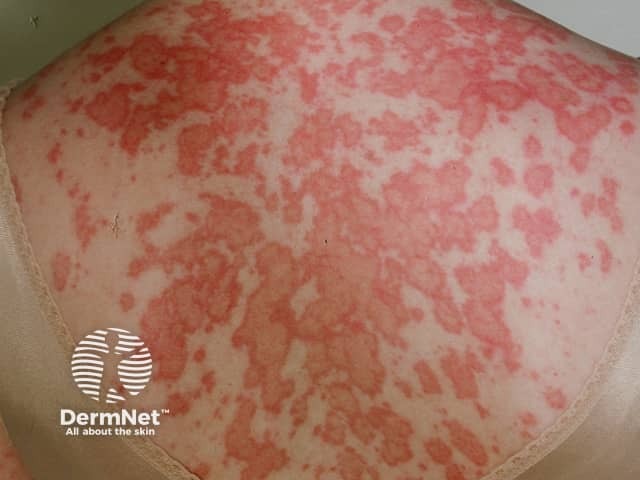
Acute cutaneous lupus erythematosus typically presents as transient erythematous patches associated with a flare of systemic lupus erythematosus.
Lupus-specific skin changes:

Malar 'butterfly' rash

Papular erythema of generalised ACLE

Sparing of knuckles
Subacute cutaneous lupus erythematosus is less commonly associated with SLE with approximately 50% having a mild form of SLE. It is thought 20–40% have drug-induced SCLE. It comprises 10–15% of cutaneous LE presentations. The skin changes are more persistent than those of ACLE.
Skin lesions of SCLE:


Intermittent CLE is better known as lupus tumidus, a dermal form of lupus erythematosus.
Skin lesions of lupus tumidus:



Lupus tumidus, smooth red nodule on the cheek
Chronic cutaneous lupus erythematosus is the most common form of CLE, and about 25% of SLE patients have some form of CCLE.
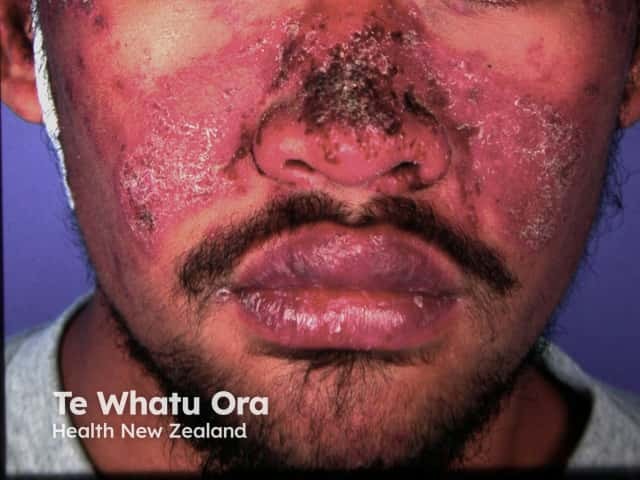
Discoid lupus erythematosus is the most common form of CCLE (80%) and is particularly prevalent and severe in patients with skin of colour. Only 1–2% of patients with localised DLE progress to SLE.
Skin lesions of DLE:

Discoid LE

Discoid lupus erythematosus

Discoid lupus erythematosus
Lupus profundus is a mostly lobular panniculitis without vasculitis.
Skin lesions of lupus profundus:


Lupus profundus

Chilblain lupus erythematosus is an under-reported form of chronic CLE involving mainly the fingers and toes of smokers triggered by exposure to a moist cold environment. It may be familial with no association to SLE, or sporadic which can be associated with SLE.
Skin lesions of chilblain lupus:

Chilblain lupus

Lupus tumidus

Some forms of cutaneous lupus erythematosus, such as bullous lupus erythematosus and discoid lupus erythematosus, are particularly associated with skin of colour.
Dyspigmentation and scarring are complications of CLE that significantly impact quality of life for patients with skin of colour.
Malar 'butterfly' rash of SLE

Discoid LE

Discoid LE with dyspigmentation and scarring

Unruly lupus hair

Cheilitis
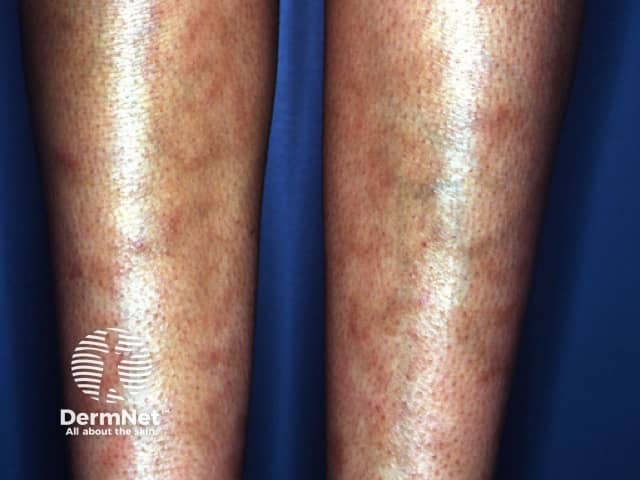
Livedo reticularis

Facial scarring and dyspigmentation of DLE

Scarring alopecia of DLE

Neonatal lupus erythematosus
The Cutaneous Lupus Erythematosus Disease Area and Severity Index scores activity and damage in each of 12 anatomical locations.
The total activity score:
Total damage score:
Cutaneous lupus erythematosus can be the presenting sign of SLE, as in acute CLE, or may evolve into SLE.
Female patients with CLE and Ro/La autoantibodies should be advised of the risk their baby may have neonatal lupus erythematosus including congenital heart block.
Chronic CLE tends to follow a chronic relapsing course for years, with flares in spring and summer, and resolution with scarring if untreated.