Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Medhir Kumawat, University of Adelaide, Australia; Dr Libby Whittaker, DermNet Medical Writer, NZ (2023)
Previous contributors: Vanessa Ngan, Staff Writer (2005)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
What is vitamin D?
Types
The relationship between vitamin D and sun exposure
Vitamin D deficiency
Vitamin D supplementation
Vitamin D in skin products
Vitamin D toxicity
Vitamin D is made up of a group of fat-soluble vitamins that exist in several forms.
The functions of vitamin D include immune protection and regulation of mineral and skeletal homeostasis.
The skin is of unique importance in the synthesis, storage, and release of vitamin D into circulation.

A vitamin D3 supplement, each contains 1000 International Units, equating to 25 mcg
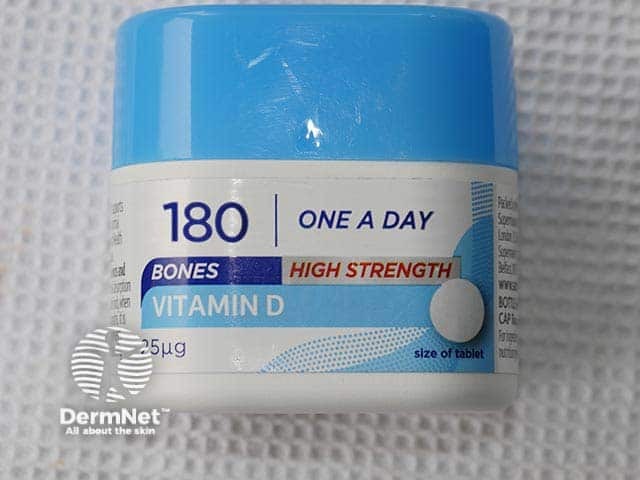
Vitamin D tablets
There are several forms of vitamin D:
Sunshine is a significant source of vitamin D, as ultraviolet B (UVB) rays from sunlight trigger vitamin D3 manufacture in the skin.
Balancing time of sunlight exposure to maintain adequate vitamin D levels, while avoiding an increased risk of sun damage and skin cancer is often discussed.
Exposure to a small amount of UV results in production of vitamin D without sunburn. Exposure to a higher amount does not result in higher amounts of vitamin D — instead, inactive luminsterol and tachysterol are produced. Exposure to large doses of UV results in sunburn with blistering and peeling.
During winter months, vitamin D production is reduced by up to 30%; the body can rely on tissue stores for 30–60 days if levels are adequate prior to winter. As summer approaches and more sunlight hours are available, more vitamin D is produced by the skin to rebuild depleted stores.
Although sunscreens could block most solar-induced production of cutaneous previtamin D3 under strictly controlled study conditions, real-life sunscreen use has not been shown to increase the risk of vitamin D deficiency (noting that some studies did not include the high-SPF sunscreens that are widely recommended today).
Risk factors for vitamin D deficiency include:
Testing for vitamin D deficiency is not always straightforward as appropriate serum levels of vitamin D vary throughout the year. The blood test is expensive and is generally not recommended unless severe deficiency is suspected.
Deficiency in vitamin D can lead to diseases including rickets and osteomalacia.
Rickets is a bone disease characterised by softening and weakening of the bones, occurring in children who are vitamin D deficient. There is a loss of calcium and phosphate from the bones, which eventually causes destruction of the supportive matrix.
In adults, vitamin D deficiency can lead to osteomalacia, which results in muscular weakness, bone pain, and bone fractures. Initially, symptoms of muscle weakness and bone pain may be subtle and go undetected.
Long-term uncorrected vitamin D deficiency can lead to osteoporosis.
In some preparations of vitamin D, dosage is quoted as micrograms; 1 microgram is equal to 40 IU.
Supplemental oral vitamin D can be taken in two forms:
Note that recommended dosing may vary in different clinical contexts and whether the aim is to treat or prevent deficiency; other appropriate clinical and pharmacological references should be consulted.
Vitamin D is also available as a combined formulation with other medications, such as calcium or bisphosphonates.
In many countries, supplemental vitamin D can be purchased over the counter, as it is generally safe and well-tolerated.
Contraindications include:
Precautions include:
Consider calcium monitoring in those receiving regular vitamin D supplementation.
Note that anticonvulsants can increase the metabolism of vitamin D and reduce its efficacy.
Vitamin D-containing skin products may be marketed for various benefits to the skin, such as reducing inflammation, improving hydration, and protecting against sun damage.
Too much vitamin D can cause toxicity that results in nausea, vomiting, low appetite, constipation, weakness, and weight loss. It can also cause hypercalcaemia, altered mental status, and cardiac arrhythmias.
Sun exposure is unlikely to result in vitamin D toxicity. Other compounds produced in the skin protect the body from synthesising too much vitamin D during prolonged sun exposure.
Vitamin D toxicity can occur from overdose of vitamin D supplements. Patients taking vitamin D should not exceed the recommended dose and be made aware of the symptoms of vitamin D toxicity to look out for.