Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, January 2016.
Introduction
Demographics and classification
Causes
Clinical features
Complications
Diagnosis
Treatment
Outlook
A mouth ulcer is damaged oral epithelium and its underlying lamina propria. Mouth ulcers are a common form of stomatitis and may be due to trauma, irritation, radiation, infections, drugs, inflammatory disorders, and unknown causes.
The most common presentation of mouth ulcers is with painful, recurrent aphthous stomatitis, also known as aphthosis, aphthae, aphthous ulcerations, and canker sores.

Aphthous ulcer

Behcet ulcer

Oral lichen planus
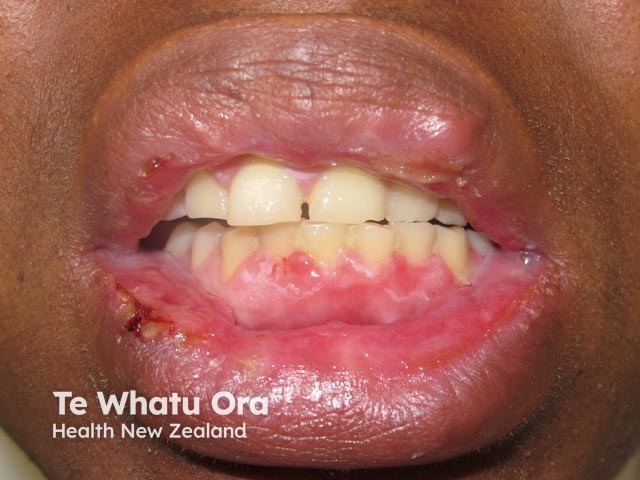
Recurrent erythema multiforme

Traumatic mouth ulcer
Males and females of all ages and races experience mouth ulcers.
Differential diagnosis includes other inflammatory disorders in which there is no true ulceration, such as migratory glossitis/geographic tongue.
Ulcers in the anterior labial sulcus

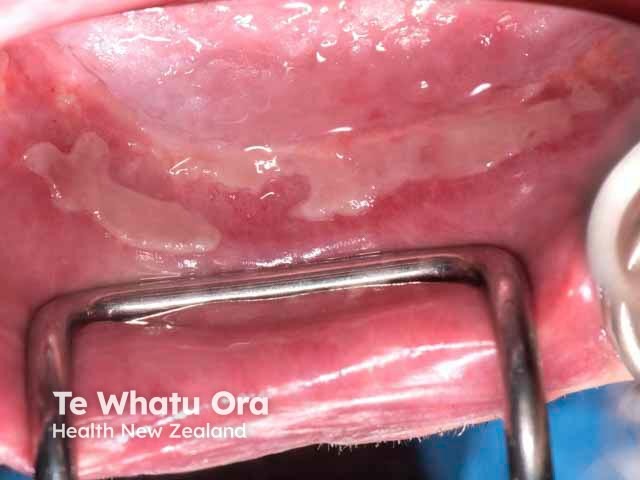
Erosions on floor of mouth
The cause or causes of aphthous mouth ulcers are not well understood. Current thinking is that the immune system is disturbed by some external factor and reacts abnormally against a protein in mucosal tissue.
Although most people with aphthous stomatitis are healthy, it may relate to:
In some patients, there are additional predisposing factors:
Patients may present to doctors or dentists with a mouth ulcer for assessment and treatment. They can also have cutaneous and systemic symptoms and signs.
A patient with a mouth ulcer should be questioned and examined with a differential diagnosis in mind.
Recurrent aphthous ulcers are divided into 3 types.
Most mouth ulcers heal without a problem.
Mouth ulcers are usually easy to diagnose. Consider biopsy of a non-healing ulcer, particularly if considering cancer. It should be taken from the indurated edge of an inflammatory ulcer or from an inflamed but non-ulcerated site.
If the patient has frequent, prolonged or large ulcers, or is unwell, the following tests may be done to assess general and gastrointestinal health.
Selected patients may undergo further assessment including endoscopy if there is suspicion of inflammatory bowel disease.
If a specific toothpaste or food is thought to precipitate ulcers, allergy tests including prick tests, patch tests and specific IgE testing may be performed. The results can be difficult to interpret.
Symptomatic relief may be obtained from:
Nicotine-containing gum has been reported to be effective, but it is not recommended because it’s highly addictive and has many adverse effects (see smoking).
Systemic therapy is intended to reduce the frequency of ulceration. A Cochrane review (2012) of systemic treatments for recurrent aphthous stomatitis was inconclusive. The following are reported to be useful in at least some patients.
Mouth ulcers are not preventable in all patients. Some people can reduce the number and severity of their ulcers by ensuring plenty of rest and avoiding known triggers.
The outlook depends on the type of mouth ulcers and their cause, if known.
There is a gradual tendency for recurrent aphthous stomatitis to become less severe in later life.