Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Updated: Hana Numan, Senior Medical Writer, New Zealand. Copy edited by Gus Mitchell. November 2021.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
Linear IgA bullous disease is a rare, autoimmune, blistering disease in which blisters form in the skin and mucous membranes including the mouth, genital mucosae, and conjunctivae.
Its name comes from the characteristic findings of linear deposition of immunoglobulin A (IgA) at the dermo-epidermal junction (at the basement membrane zone), which is demonstrated by immunofluorescence. It is also called linear IgA bullous dermatosis and in children, it may be known as linear IgA dermatosis of childhood or chronic bullous disease of childhood.

Blisters on the leg in Linear IgA disease

'String of beads' sign in a child with linear IgA disease

Symblepharon in linear IgA disease
Linear IgA bullous dermatosis is rare; the annual incidence in some countries is reported to be approximately 0.5–2 cases per million people. It can occur in both adults and children.
In adults, disease onset is more common in the sixth decade. In children, disease onset is more common during preschool age (~4.5 years old).
It has been suggested that it may be more common in children in developing countries.
Linear IgA bullous disease can be associated with some underlying diseases such as inflammatory bowel disease (Crohn, ulcerative colitis), solid and lymphoid malignancies, and rheumatoid arthritis. Unlike dermatitis herpetiformis, where the deposits of IgA on direct immunofluorescence are granular, there is no association with gluten sensitive enteropathy.
Extremely rarely, severe IgA bullous disease develops in the neonatal period, and may progress to produce severe mucosal, aerodigestive lesions, and corneal scarring. It may be due to pathogenic IgA in breast milk, and breast feeding should be discontinued.
Linear IgA bullous dermatitis can be idiopathic or drug-induced. Although it is known to be an autoimmune disease, the exact mechanism of lesion development is not well understood.
Genetic involvement may contribute to the development of chronic bullous disease of childhood where a number of human leukocyte antigen types have been linked.
Drug-induced IgA disease usually resolves on withdrawal of the offending drug. Drugs that may be implicated include:
Linear IgA bullous disease may present as toxic epidermal necrolysis (TEN) — a severe cutaneous adverse drug reaction with widespread blistering and painful loss of skin. A few cases have been described in which direct immunofluorescence has revealed characteristic linear deposits of IgA.

Linear IgA

Linear IgA

Linear IgA

Palmar blisters

String of beads sign

Chronic bullous disease of childhood
Eye involvement may result in irritation, dryness, photosensitivity, blurred vision, corneal scarring, and even blindness.
History and examination is usually not enough to give a definitive diagnosis as clinical signs and symptoms often resemble other blistering conditions.
Linear IgA bullous disease is best diagnosed by performing direct immunofluorescence of skin adjacent to a blister; it reveals a linear band of IgA at the dermo-epidermal junction.
A thorough medication history should also be taken to determine possible drug aetiology.
Other tests that may be used include:
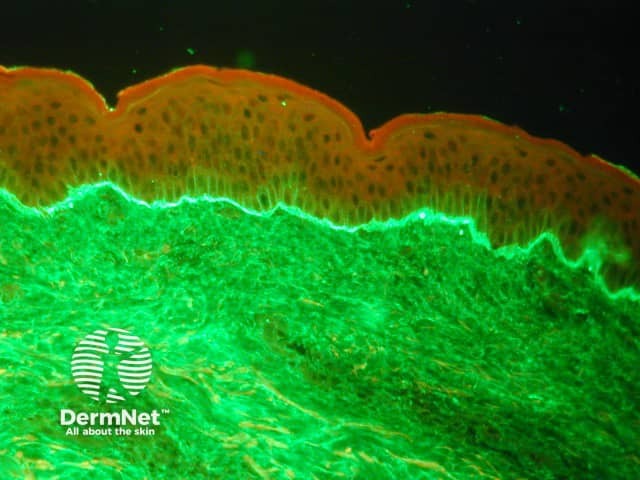
Linear deposit of IgA at the dermoepidermal junction on direct immunofluorescence
Linear IgA bullous disease usually improves or clears when treated with dapsone, an immunomodulatory sulphone. Its success as treatment is well-established and improvement can usually be seen within just 2 to 3 days of drug initiation.
Other medications that have been used to treat linear IgA disease include:
Linear IgA bullous disease generally has a good prognosis. Approximately 30–60% of adult patients experience spontaneous remission but usually only after years of disease. In children, spontaneous disease remission usually occurs after 2–4 years of disease onset.
However in some patients, long-term treatment may be required if reduction in dose of active treatment results in further blistering.
Drug-induced linear IgA disease has good outcomes where remission occurs in most cases within 2–6 weeks of discontinuation of the offending drug.