Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Connective tissue diseases
Created 2009.
Learning objectives
- Recognise cutaneous connective tissue diseases
Introduction
The so-called connective tissue diseases are the result of environmental stimuli (such as drugs, infection or exposure to ultraviolet radiation) in genetically predisposed individuals. They are associated with a range of circulating autoantibodies.
Lupus erythematosus
- All varieties of lupus erythematosus (LE) are more common in females than in males. They are uncommon in children and most often arise in those with coloured skin.
- Discoid LE is the most common presentation and results in red scaling plaques on light-exposed areas especially the face and scalp. The plaques heal with scarring. Discoid lupus in children is more likely than in adults to progress to systemic disease.
- Subacute cutaneous LE is characterised by more widespread photosensitive annular plaques. This type of LE may occur in the mothers of babies with neonatal LE (or they may appear healthy).
- Positive anti-Ro antibodies are characteristic of subacute cutaneous LE, and mothers of babies with neonatal LE.
- Neonatal LE presents at birth or within the first 3 months, with photosensitive, dry, annular, erythematous plaques mainly on the head and neck. These resolve within 6 to 12 months. Congenital complete heart block, hepatic and haematological involvement may also occur.
- Treatment of cutaneous LE in older children and adults includes sun protection, potent topical steroids, antimalarials and a variety of immunosuppressive treatments.
Cutaneous lupus erythematosus without systemic disease
Severe discoid LE Subacute cutaneous LE 

Systemic lupus (SLE) is characterised by:
- A“butterfly” macular facial rash
- Photosensitivity
- Patchy hair loss
- Palmar erythema
- Periungual telangiectasia.
- Systemic symptoms, including fever (>90%), fatigue (>90%), arthritis, CNS, renal, cardiac and pulmonary disease.
Drug-induced lupus may be due to a variety of antibiotics (in adolescents, most often minocycline), antihypertensive and anti-inflammatory medications.
Cutaneous signs of lupus erythematosus

Butterfly rash

Discoid lupus
Dermatopathological findings in SLE include a lichenoid tissue reaction and a band of immunoglobulins at the dermo-epidermal junction (detected by direct immunofluorescence of clinically involved skin).
Dermatopathology of systemic lupus erythematosus This shows a dense perivascular and periadnexal lymphocytic inflammatory infiltrate and interface changes with vacuolar degeneration of basal layer
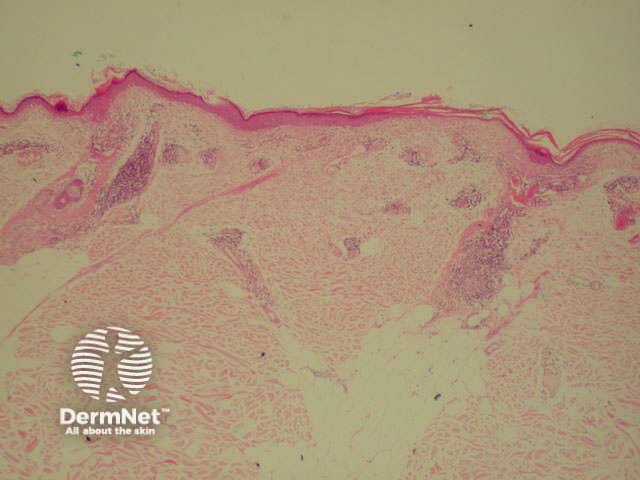
Low power view
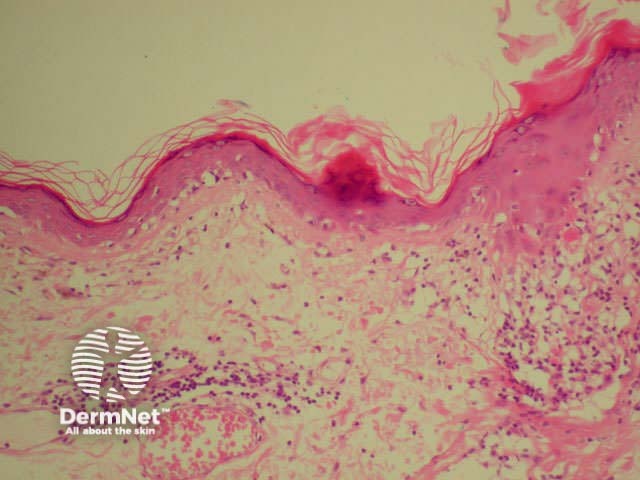
Medium-powered view
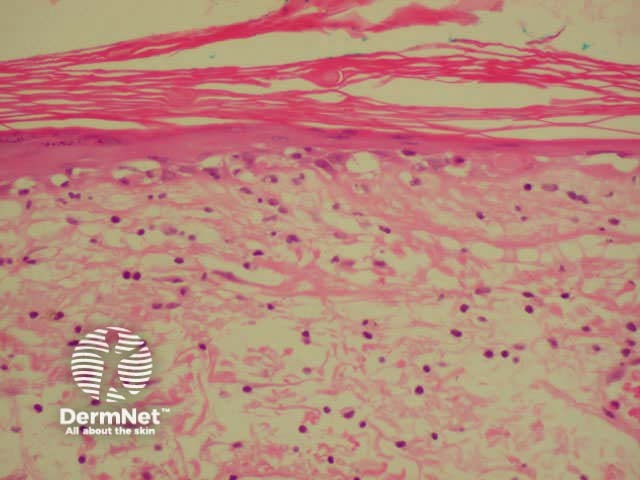
High-power view
Investigations should include:
- CBC (anaemia, leucopaenia, thrombocytopenia suggest SLE)
- ESR (reflects activity of SLE)
- Urinalysis (proteinuria and casts in renal lupus)
- Auto-antibodies including ANA (positive in >90% of SLE), ENA, anti-double-stranded DNA
- Lupus anticoagulant
- Complement profile
Scleroderma
Scleroderma (tight skin) is seen in the following conditions:
- Morphoea
- Raynaud disease (Raynaud without known underlying disease)
- Systemic sclerosis
- Mixed connective tissue disease
- Scleroedema
- Chronic graft versus host disease
Morphoea
Morphoea is characterised by ivory white oval sclerotic plaques with an inflamed edge that eventually result in post-inflammatory pigmentation and dermal or subcutaneous atrophy. It is not uncommon in children and adolescents.
A linear variety can involve underlying muscle and bone and is more common in children. If it affects the face and /or scalp, it is also known as en coup de sabre.

Morphoea

Linear morphoea

En coup de sabre
Systemic sclerosis
Systemic sclerosis is characterised by progressive accumulation of collagen, fibrosis and loss of mobility of the skin and other organs such as the respiratory and gastrointestinal tracts. it is exceedingly rare in children
The CREST variant (Calcinosis, Raynaud's, oEsophageal, Sclerodactyly, Telangiectasia) may have less severe systemic manifestations.
Treatment is mainly symptomatic at this time.

Severe digital resorption

CRST syndrome

Calcinosis cutis
Chronic graft-versus-host disease (GVHD)
- GVHD arises more than 100 days after bone marrow transplantation and affects 25% of survivors
- It may result in generalised scleroderma, lichen planus-like papules and lichenoid histology.
Dermatomyositis
- Dermatomyositis can be seen in children and adults.
- It is sometimes associated with malignancy, especially in those over 55 years of age (malignancy is very rare in children).
- It presents with muscle weakness, elevated muscle enzymes and a rash affecting the face, chest, arms and hands
- Dermatomyositis of the eyelids is known as heliotrope rash.
- Violaceous plaques over the knuckles are known as Gottron's papules.
- Calcinosis cutis is particularly common in juvenile dermatomyositis.

Heliotrope rash

Gottron papules
Rheumatoid arthritis
Systemic-onset juvenile rheumatoid arthritis is sometimes associated with an evanescent salmon-pink rash on the trunk. Rheumatoid nodules, vasculitis and leg ulcers are more common in adults with rheumatoid disease.
Rheumatic fever
- Autoimmune reaction to Group A streptococcal pharyngitis
- Clinical criteria for diagnosis are fever, migratory polyarthritis, carditis and Sydenham's chorea.
- Erythema marginatum is characterised by erythematous, gyrate, non-scaly annular plaques or macules that migrate centrifugally.
Activity
Describe the management of cutaneous lupus erythematosus in pregnancy.
References:
On DermNet:
Information for patients
Other websites:
- Medscape Reference:
- Connective tissue diseases
- Rheumatology (paediatrics)
Books about skin diseases:
See the DermNet bookstore
