Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Autoimmune/autoinflammatory Diagnosis and testing
Author: Dr Ben Tallon, Dermatologist/Dermatopathologist, Tauranga, New Zealand, 2011.
Scanning power of lichen sclerosus reveals a lichenoid inflammatory pattern in early stage lesions or a superficial sclerosing process in late stage lesions (Figure 1 and 2). The epidermis shows hyperkeratosis, significant thinning with loss of the normal rete ridge pattern and plugging of follicular infundibulae (Figure 3). An atrophic epidermis is not a requirement as some cases particularly in the vulva can show significant epidermal hyperplasia. Vacuolar degeneration of the basal layer can be seen though typically mild especially in late stage lesions. Clefting can be evident between the epidermis and dermis as a result of this basal layer degeneration and the underlying dermal changes. The dominant feature is of broad condensation of the dermal collagen. These changes are typically superficial, while in early lesions may show marked overlying papillary dermal oedema. When extending into the deep dermis discrimination from scleroderma may become difficult. The inflammatory infiltrate evolves from a dense lichenoid lymphocytic infiltrate to a sparse superficial interstitial infiltrate in late stage disease. Scattered plasma cells, histiocytes and mast cells can be seen (Figure 4).
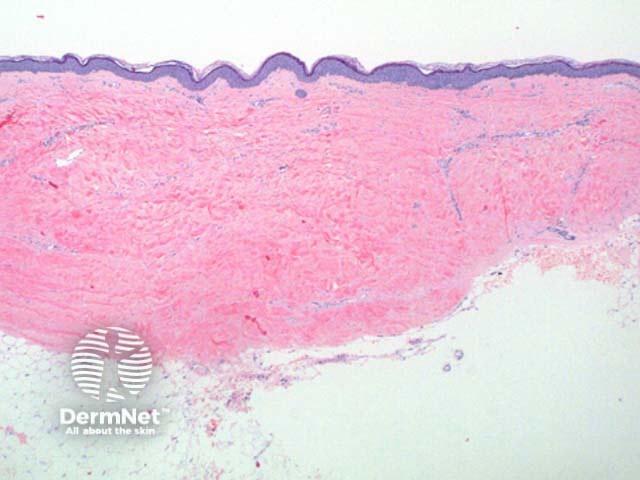
Figure 1
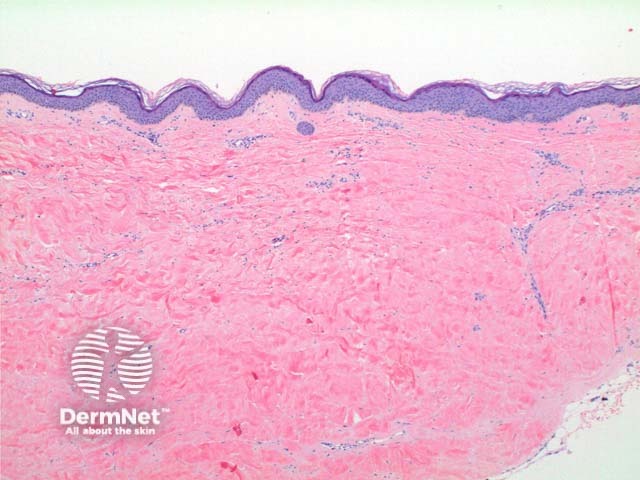
Figure 2
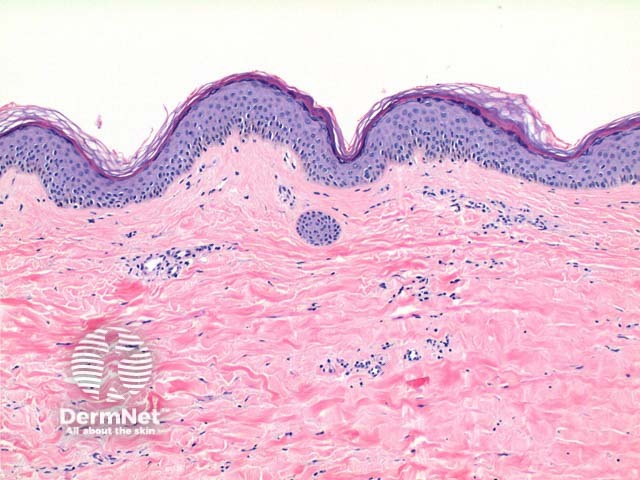
Figure 3
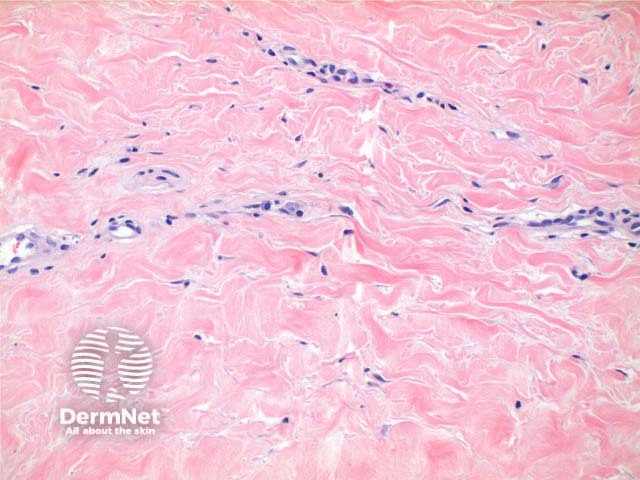
Figure 4
Scleroderma: In this condition the overlying epidermis and superficial dermis is spared. The inflammatory infiltrate is typically sparse and around deep adnexal and vascular structures. Overlap can occur where superficial and deep changes co-exist.
Lichen planus: The presence of a well formed granular layer and numerous cytoid bodies, and a lack of basement membrance thickening or epidermal atrophy favour lichen planus over lichen sclerosus.