Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lipoedema – therapy — extra information
Lipoedema – therapy
Author:Dr Axel Baumgartner, General Surgeon and Director of the Hanse-Klinik, Lübeck, Schleswig-Holstein, Germany. September 2020. Copy edited by Gus Mitchell. October 2020.
What is the treatment for lipoedema?
Treatment for lipoedema (American spelling lipedema) comprises several measures depending on the disease stage. In addition to conservative therapies, surgical treatment has also become well established.
General measures
Patients should maintain an active lifestyle including appropriate exercise depending on their individual limits and while wearing compression garments. A balanced diet is required to avoid becoming overweight or to reduce obesity. Psychological support should be offered.
Conservative measures
The goal of conservative treatment is to reduce the volume of interstitial fluid. In the early stages of lipoedema, manual lymph drainage is not absolutely necessary. In many cases, having the legs in a horizontal position while sleeping is enough to enable absorption of the fluid.
Orthostatic oedema can be prevented with compression stockings. Round-knit compression garments, at least as a thigh-high stocking and preferably as pantyhose, are initially sufficient. The garment must not constrict any part of the leg.
Patients with irreversible orthostatic oedema and increasing amounts of fatty tissue must commence lifelong complete physical decongestive therapy (CDT) (Fig. 1). CDT includes therapy with regular lymph drainage, either manually or with a lymphatic drainage machine, and the wearing of flat-knit compression garments.
Orthostatic oedema complicating lipoedema

What is the surgical treatment of lipoedema?
Since 2005, surgical treatment with liposuction has been included in the lipoedema treatment guidelines in Germany. By reducing the pathologically increased volume of subcutaneous fat, the patient’s symptoms are significantly improved.
Indications
In addition to reducing volume in patients with lipohypertrophy (local fatty tissue proliferation without swelling-related complaints) with cosmetic impairment, liposuction is gaining importance as a medically indicated intervention. The procedure is increasingly used in individual patients to reduce volume in cases of severe fatty tissue proliferation resulting from primary or secondary lymphoedema. It is also suitable for male breast reduction.
However, the main medical indication for liposuction is for the treatment of lipoedema.
Techniques
A number of different liposuction techniques are used, including laser-assisted, radiofrequency-assisted, and ultrasound-assisted liposuction. However, since the introduction of tumescent local anaesthesia (TLA), the predominant techniques used for medical liposuction are power-assisted liposuction (PAL) using vibrating blunt suction cannulas, and water jet-assisted liposuction (WAL). PAL and WAL have reduced risks for patients and are less disruptive to the tissue and lymphatics.
Water jet-assisted liposuction (WAL)
With water jet-assisted liposuction, a thin, high-energy water jet is used to detach the fat cells from the surrounding tissue and simultaneously suction them. This eliminates the need to infiltrate large quantities of TLA prior to liposuction, which is easier on the body.
Tumescent local anaesthesia and power-assisted liposuction (TLA+PAL)
Tumescent local anaesthesia is a technique of infiltrating the subcutaneous fatty tissue with large volumes of diluted anaesthetic. With TLA, liposuction can be performed without general anaesthesia. The high tissue pressure achieved with the procedure loosens the fatty tissue. This “softening effect” allows the use of thin (3 to 4 mm) blunt suction tips with small laterally placed apertures. The procedure is gentle and retains the connective tissue scaffolding of the subcutaneous tissue.
With power-assisted liposuction (PAL), the vibrating cannula tip (4,000 vibrations per minute) glides past the connective tissue structures without them being suctioned into the cannula. This significantly reduces the shearing forces and the fatty tissue “loosened” by the TLA solution enters the cannula more easily.
Before surgery
Before deciding on treatment with liposuction, examination focuses on the composition and extent of the fatty tissue for surgery planning. During the consultation, the patient is informed about the risks associated with liposuction and receives a realistic assessment of the anticipated final results. Imaging is required only in exceptional cases.
Immediately prior to liposuction, photographic documentation is performed, the sites to be operated on are marked, and the TLA solution is infiltrated.
During surgery
Suction is performed through several 4 mm incisions made at sites that are as inconspicuous as possible. The cannula tip is guided along the longitudinal axis, which is easier on the lymphatic network in the subcutaneous fatty tissue.
After surgery
Directly after the procedure, the patient is asked to stand up to evaluate the results. The wound edges are not sutured; the wound is later closed with a fluid-permeable adhesive strip. The solution, which drains most profusely in the hours following the procedure, is captured with pads under the compression girdle. Moderate drainage of the fluid continues for another 2 or 3 days.
Deep venous thrombosis prophylaxis is recommended for at least 5 days.
Patients are instructed to wear a compression girdle composed of an elastic material for at least 4 weeks. In addition, postoperative manual lymph drainage reduces temporary swelling. Patients are mobile after the procedure and should keep moving.
Contraindications
Contraindications for liposuction concern possible adverse effects of the local anaesthetic used for TLA, such as allergic reactions or intolerance, rather than the procedure itself. Since the local anaesthetic can influence the electrical conduction of the heart, patients with heart failure and arrhythmia should not be treated.
Liposuction is also contraindicated for general abdominal obesity and dysmorphophobia (pathological dislike of part of one’s own body).
What are the complications of liposuction?
Adverse effects that typically occur as part of the wound healing process include sore muscles (similar to post-exercise soreness), temporary swelling, temporary sensory changes to the surface of the skin, and tissue hardening in the weeks following liposuction. Extensive bruises and wound infections are rare. The frequency and extent with which indentations will occur, skin abnormalities, and asymmetry depend on the surgeon’s experience, as well as on the patient’s condition prior to surgery and the consistency of the tissue.
The risk of blood clot is reported as between 0.05 to 0.1%. Patients with the following risk factors are particularly at risk of blood clot: being overweight, oral contraceptives, smoking, and hereditary coagulation disorders.
Lymphatic damage resulting in subsequent secondary lymphoedema is not observed either clinically or experimentally following PAL or WAL.
When performed by an experienced surgeon, complications from liposuction are rare.
What is the outcome following lipoedema surgery?
The persistence of cosmetic and symptomatic improvements achieved by liposuction has been confirmed in a long-term study. In addition to a reduction in the pathologically increased fat deposits with normalisation of body proportions (Fig. 2a,b), there was a marked improvement in clinical symptoms, which showed significant pre- and post-operative differences. Following liposuction, 40% of women reported no longer needing lymph drainage, and 60% had a reduced requirement.
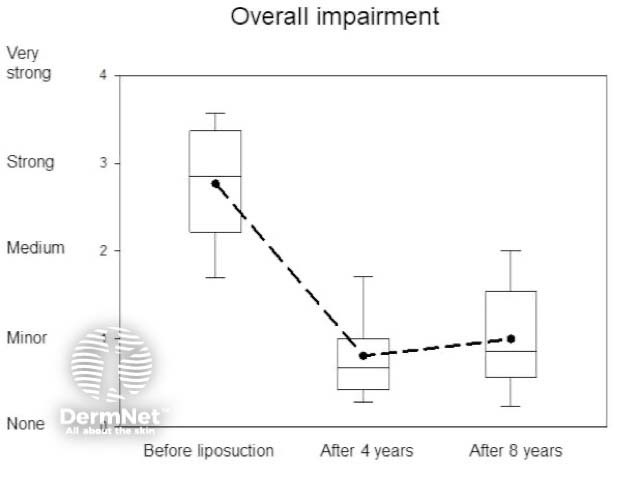
Spontaneous pain and tenderness, oedema formation, tendency to bruise easily, reduced mobility, and cosmetic disfigurement decreased, with subsequent improvement in the quality of life. The overall impairment of these female patients measured by these parameters is shown in Fig. 3, which shows the reduction over time as box plots before and an average of 4 and 8 years after liposuction. The sub-test 'overall impairment' is considered to be a particularly reliable value for measuring treatment success. Lower values indicate less discomfort and thus better well-being. All descriptions after liposuction indicate an improved condition after the intervention.
The reduction in fat deposits on the inner thighs and knees also led to a decrease or total elimination of mechanical and occlusion-related skin damage. The pseudo-X leg position caused by the increased adipose tissue present in some patients was also reduced or abolished.
Overall impairment before and after liposuction


Based on its efficacy and long-lasting results, the surgical removal of fat, together with combined physical decongestive therapy, is an essential part of treatment for lipoedema. The only way to achieve long-lasting results is to use a combination of all of the treatment measures described above.
References
- Peprah K, MacDougall D. Liposuction for the Treatment of Lipedema: A Review of Clinical Effectiveness and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2019 Jun 7. PMID: 31479212. PubMed
- Reich-Schupke S, Schmeller W, Brauer WJ, Cornely ME, Faerber G, Ludwig M, Lulay G, Miller A, Rapprich S, Richter DF, Schacht V, Schrader K, Stücker M, Ure C. S1 guidelines: Lipedema. J Dtsch Dermatol Ges. 2017 Jul;15(7):758–67. doi: 10.1111/ddg.13036. PMID: 28677175. PubMed
- Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema-results of a study with 25 patients. J Dtsch Dermatol Ges. 2011 Jan;9(1):33–40. English, German. doi: 10.1111/j.1610-0387.2010.07504.x. Epub 2010 Sep 7. PMID: 21166777. PubMed
- Schmeller W, Hueppe M, Meier-Vollrath I. Tumescent liposuction in lipoedema yields good long-term results. Br J Dermatol. 2012 Jan;166(1):161–8. doi: 10.1111/j.1365-2133.2011.10566.x. Epub 2011 Nov 17. PMID: 21824127. PubMed
- Brorson H. Liposuction in Lymphedema Treatment. J Reconstr Microsurg. 2016 Jan;32(1):56–65. doi: 10.1055/s-0035-1549158. Epub 2015 Apr 20. PMID: 25893630. PubMed
- Coleman WP 3rd. Powered liposuction. Dermatol Surg. 2000;26(4):315–18. doi:10.1046/j.1524-4725.2000.99240.x. Journal
- Hoffmann JN, Fertmann JP, Baumeister RG, Putz R, Frick A. Tumescent and dry liposuction of lower extremities: differences in lymph vessel injury. Plast Reconstr Surg. 2004 Feb;113(2):718–24; discussion 725–6. doi: 10.1097/01.PRS.0000101506.84361.C9. PMID: 14758241. PubMed
- Stutz JJ, Krahl D. Water jet-assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic Plast Surg. 2009 Mar;33(2):153–62. doi: 10.1007/s00266-008-9214-y. Epub 2008 Jul 29. PMID: 18663515. PubMed
- Baumgartner A, Hueppe M, Schmeller W. Long-term benefit of liposuction in patients with lipoedema: a follow-up study after an average of 4 and 8 years. Br J Dermatol. 2016 May;174(5):1061–7. doi: 10.1111/bjd.14289. Epub 2015 Dec 26. PMID: 26574236. PubMed
On DermNet
