Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Myofibroma pathology — extra information
Lesions (benign) Diagnosis and testing
Myofibroma pathology
Author: Dr Ben Tallon, Dermatologist/Dermatopathologist, Tauranga, New Zealand, 2011.
Histology Special stains Histological variants Differential diagnoses
Myofibroma is a benign fibrous tumour. It is most commonly a solitary lesion arising in the first 2 years of life, when it is also called solitary infantile myofibroma. It is thought to be of myofibroblastic origin.
Histology of myofibroma
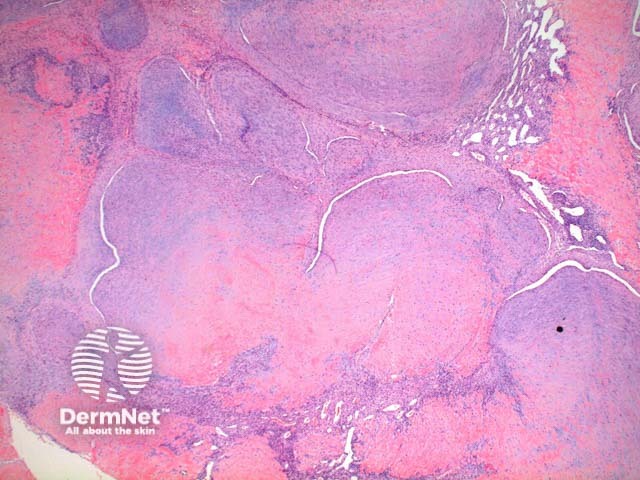
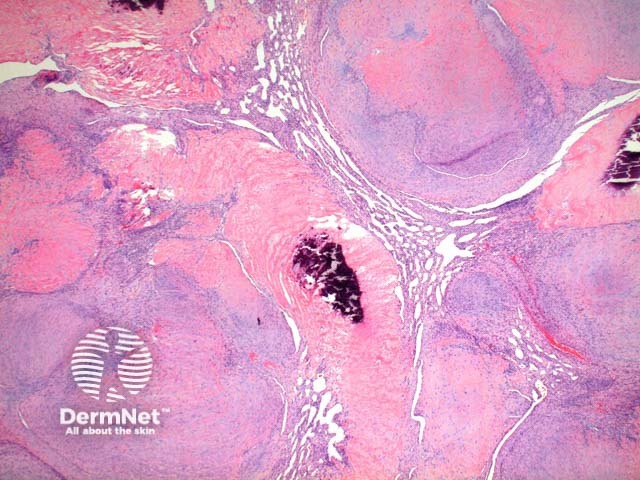
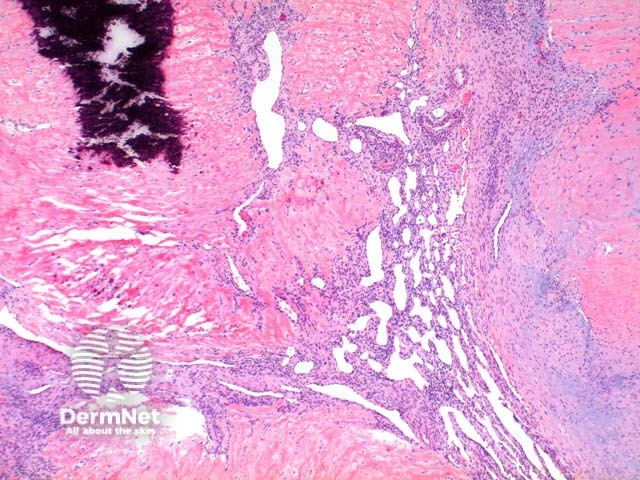
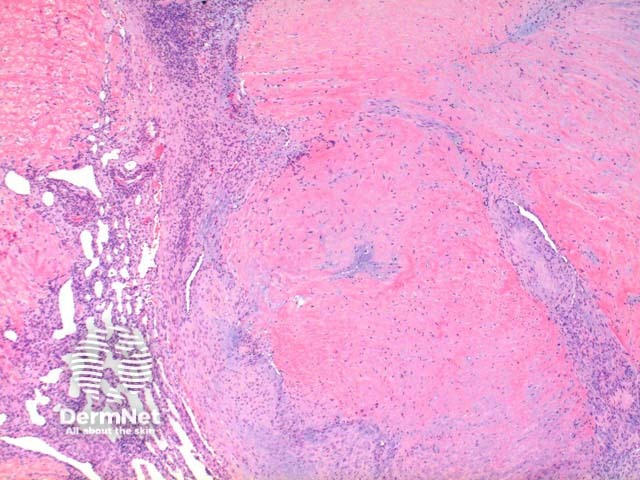
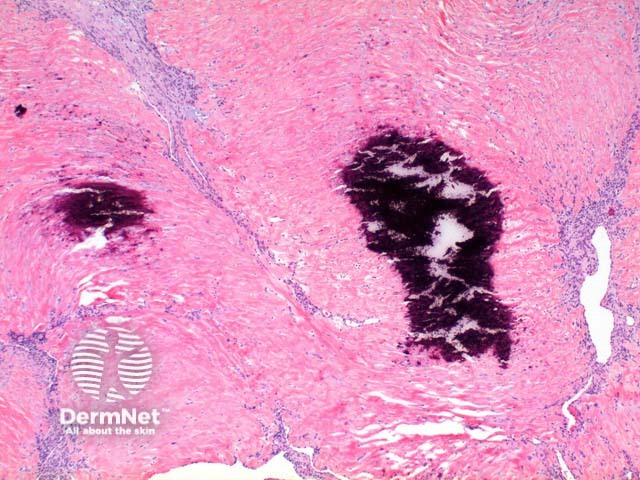
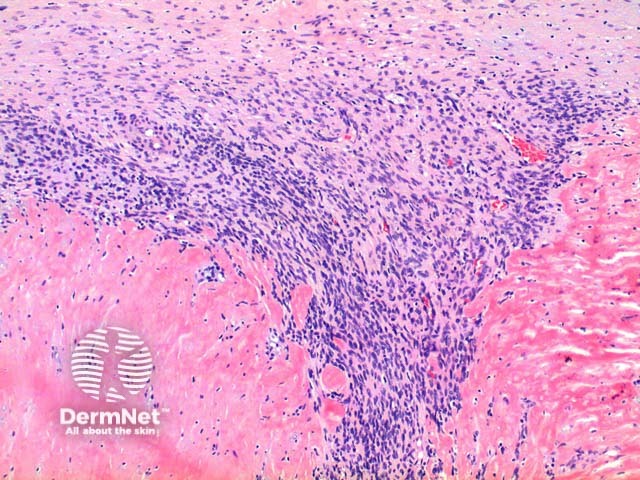
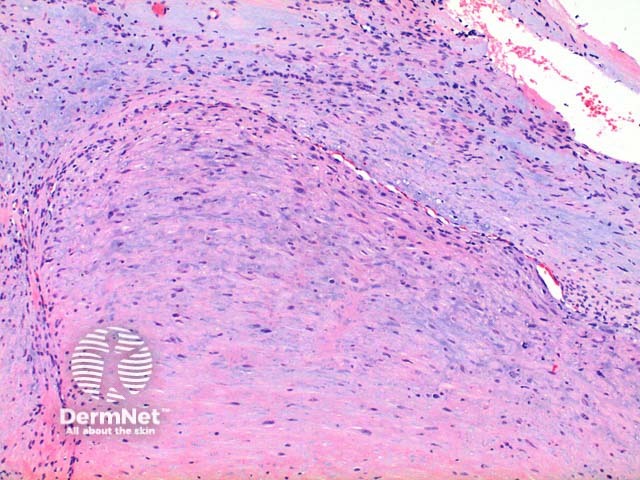
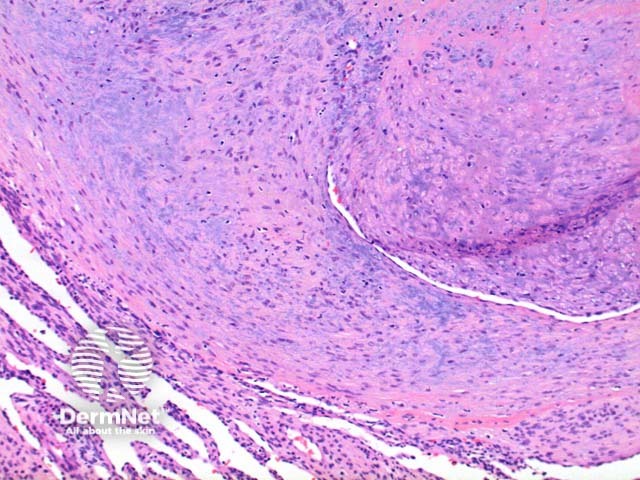
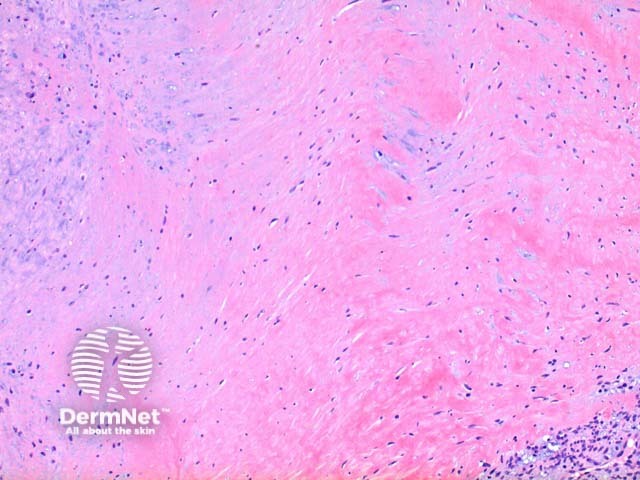
Low power view of myofibroma demonstrates a well defined multinodular tumour arising in the deep dermis or subcutis (Figure 1). Also at low power a branching ‘staghorn’ like pattern of blood vessels can be seen between the tumour nodules (Figure 2). Areas of calcification can often be seen (Figures 2, 3 and 5). The tumour nodules are comprised of a spindle cell proliferation with short plump nuclei (Figures 4,5 and 6). A basophilic tinge in the spindled peripheral component of the nodules is evident (Figures 7 and 8). Sclerotic collagen in the centre of the tumour nodules gives a biphasic appearance to the tumour (Figure 9).
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Myofibroma pathology
Special stains in myofibroma
Typically the spindle cell component of myofibroma stains positively to vimentin and smooth muscle actin, with variable staining seen to desmin.
Histological variants of myofibroma
A small number of clinical myofibroma variants exist.
Solitary cutaneous myofibromas: Solitary lesions arising in adults.
Multiple congenital myofibromas: May be seen with or without systemic involvement. Visceral involvement portends a poor prognosis.
Differential diagnosis of myofibroma
Myopericytoma: There is significant overlap with this tumour and they may fall along a spectrum. A concentric perivascular proliferation favours myopericytoma, whereas a biphasic appearance with hyalinised paucicellular areas favours myofibroma.
References
- Skin Pathology (3rd edition, 2002). Weedon D
- Pathology of the Skin (3rd edition, 2005). McKee PH, J. Calonje JE, Granter SR
- Granter SR, Badizadegan K, Fletcher CDM. Myofibromatosis in adults, glomangiopericytoma, and myopericytoma. A spectrum of tumors showing perivascular myoid differentiation. Am J Surg Pathol. 1998;22:513–25. PubMed
On DermNet
