Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Senile purpura — extra information
Senile purpura
Author: Ken Hiu-Kan Ip, Medical Student, University of Auckland. Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton New Zealand. February 2014.
Introduction Demographics Clinical features Causes Diagnosis Management Prognosis
What is senile purpura?
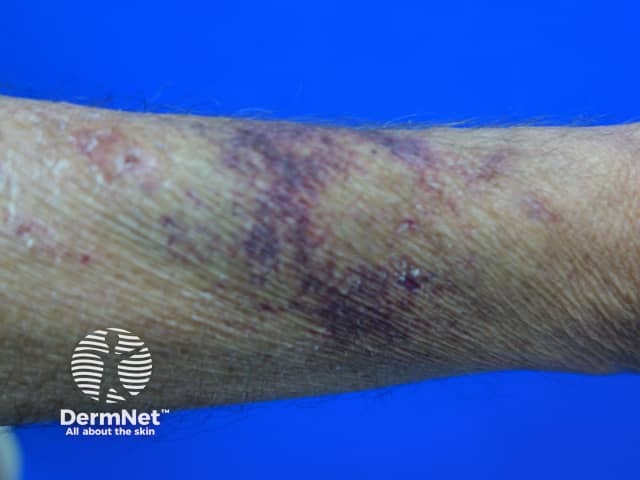
Senile purpura is a common, benign condition characterised by the recurrent formation of purple ecchymoses (bruises) on the extensor surfaces of forearms following minor trauma.
It is also known as Bateman purpura, after British dermatology pioneer Thomas Bateman, who first described it in 1818; and actinic purpura, because of its association with sun damage.
Senile purpura

Senile purpura

Senile purpura

Senile purpura

Senile purpura

Senile purpura
Who is at risk of senile purpura?
Senile purpura affects over 10% of those aged over 50 years old. It is equally common in males and females.
Other risk factors include chronic sunlight exposure and the use of oral or topical corticosteroids and anticoagulants (blood thinners).
What are the clinical features of senile purpura?
Senile purpura is characterised by irregularly-shaped macules, 1 – 4 cm in diameter, that are dark purple with well-defined margins. The lesions do not undergo the colour changes of a bruise and take up to three weeks to resolve.
The surrounding skin is typically thin, inelastic and pigmented in association with others signs of skin ageing and sun damage.
The lesions are most commonly distributed on the extensor surface of forearms and dorsal aspect of hands. Infrequently, they also occur on necks and faces.
The patient may recall minor blunt trauma to skin preceding the appearance of the lesions. They may also note multiple similar lesions which have appeared in the past but now resolved.
What causes senile purpura?
With age and photodamage, the dermal tissues become thin and increase the fragility of blood vessels. As a result, superficial vessels tear and rupture even with negligible trauma. The subsequent extravasation of blood into the surrounding dermis results in the development of dark purple ecchymoses.
Persistent brown pigmentation following the resolution of the bruises results from the deposition of haemosiderin, a component of red blood cells.
How is senile purpura diagnosed?
Senile purpura can be diagnosed based on clinical appearance alone.
Histologically, the epidermis is thinned, and the dermis demonstrates significantly reduced amounts of collagen replaced by abnormal elastic fibres, as well as extravasated red blood cells. The vessel walls of the dermis are normal in structure.
Coagulation studies are rarely necessary and will typically be unremarkable.
What is the management of senile purpura?
Senile purpura is benign and self-resolving.
Patients should be educated on sun protection measures, including sunscreen application and sun-protective clothing to protect their skin from further photodamage.
What is the prognosis?
Although cosmetically displeasing, senile purpura is benign and unrelated to any systemic diseases or blood dyscrasias. It is, however, a risk factor for skin tears in institutionalised patients.
The purpuric lesions resolve over one to three weeks and may produce residual brown pigmentation of the skin. Unfortunately, senile purpura is recurrent and associated with lifelong reappearance of new lesions.
References
- Tattersall RN, Seville R. Senile purpura. QJM. 1950:19 (2): 151–9. Journal
- Beauregard S, Gilchrest BA. A survey of skin problems and skin care regimens in the elderly. Arch Dermatol. 1987:123 (12); 1638. PubMed PMID: 3688904.
- Ratliff CR, Fletcher KR. Skin tears: a review of the evidence to support prevention and treatment. Ostomy Wound Manage. 2007:53 (3); 32–42. Pubmed PMID: 17395986.
On DermNet
