Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2009.
Hair loss may refer to excessive shedding or baldness (or both). Balding can be localised or diffuse, scarring or non-scarring. Increased hair can be due to hormonal factors (hirsutism) or non-hormonal (hypertrichosis). Scalp disorders may or may not be associated with hair loss.
Shedding is most often temporary and due to telogen effluvium (hair bulbs present), but may also be during anagen (no hair bulb) if due to alopecia areata or provoked by a drug (e.g. retinoid, hormone, anticoagulant, statin, cytotoxic).
Telogen effluvium may follow two or three months after a provoking event, most often parturition, sudden weight loss, blood loss, fever or stress. The shedding stops within a few months but it may take a couple of years for the hair bulk to appear normal.
Chronic telogen effluvium arises when the hair cycle has sped up so that the anagen phase is shorter; identify and treat iron deficiency (test ferritin) and hypothyroidism. it is rare in children; most cases are women with diffuse non-androgenic pattern balding.
Telogen effluvium Telogen effluvium 

Diffuse hair thinning in adults is most often due to male pattern balding in men (androgen-dependent) and female pattern balding (non-androgen-dependent) in females. These rarely present in adolescents. However, diffuse hair thinning may accompany internal disease (particularly systemic lupus erythematosus and syphilis). Thin fragile hair may also accompany iron deficiency. Coarse dry hair may be due to hypothyroidism. In the absence of other symptoms, alopecia areata may be responsible.
Pattern balding (male) Pattern balding (female) 

Balding can be reversible, but if there is scarring it is permanent. Alopecia areata is the most common cause of one or more areas of localised baldness on the scalp and other hair-bearing areas. It is an autoimmune skin disease and is more common in those affected by, or with a family history of, vitiligo, diabetes and thyroid disease. It is also more common in Down syndrome. Although the onset may be at any age, it most often starts in childhood or young adult life.
The scalp appears normal in alopecia areata, but there may be broken-off short hairs resembling exclamation marks (!) In typical alopecia areata, there are one or several round smooth bald patches. In about 5% all hair from the head is lost (alopecia totalis) and in 1% the body hair is also lost (alopecia universalis). In 80% there is regrowth within a few months, but it may be lost elsewhere at the same time or later. Prognosis seems less good in very young children, if the initial hair loss is severe and extensive or affecting facial areas. The nails may be affected resulting in pitting and ridging.
Alopecia universalis Loss of eyebrows Marginal regrowth Improvement 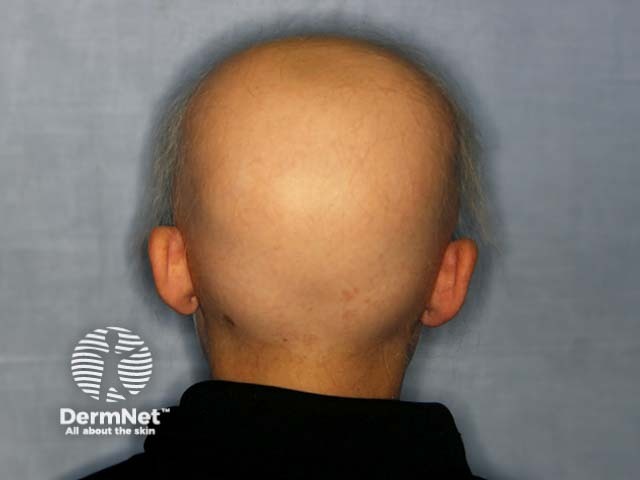



There is a strong placebo effect of treatment because spontaneous regrowth may occur at any stage. It is therefore hard to assess the value of individual treatments. Limited localised disease in children is best managed by ultrapotent topical steroid cream or gel under occlusion. Older children may tolerate intralesional corticosteroid injections 6 to 8-weekly (maximum 20mg per visit).
District Health Boards provide a subsidy to obtain a wig, if medically necessary.
If bald patches are accompanied by inflammation (erythema, scaling, pustules) consider other reasons for hair loss in children:

Tinea capitis

Trichotillomania
These disorders may result in scarring (cicatricial alopecia) in which there is shiny pale skin and reduced or absent follicular orifices.
These are rare and diagnosed by light or electron microscopy. They present as thin, short, or unruly hair in young children. The most common abnormalities are:

Loose anagen syndrome
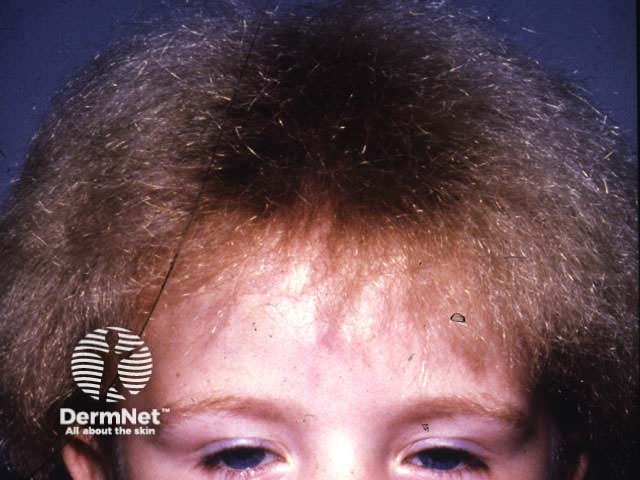
Spangled hair shaft abnormality
Skin diseases that favour the scalp may not cause any hair loss, although when they are very severe this may occur.
The most common conditions affecting the scalp are:
| Dandruff or pityriasis capitis | Diffuse scaling |
| Seborrhoeic dermatitis | Ill-defined inflammatory plaques with yellowish scale |
| Psoriasis | Diffuse or localised well-defined erythematous plaques with silvery scale |
| Pityriasis amiantacea | Sticky scale due to underlying psoriasis or seborrhoeic dermatitis |
| Head lice | Adult lice, nits on hair shaft, tiny haemorrhagic spots and excoriations |
| Lichen simplex | Well demarcated lichenified intensely itchy plaques, usually on occiput |
| Folliculitis | Chronic scattered and irritable follicular pustules |

Pityriasis amiantacea

Infantile seborrhoeic dermatitis

Scalp folliculitis
Hirsutism is excessive hair growth in females in the beard area, around the nipples, in a male pattern on the abdomen (diamond-shaped pubic hair) and often elsewhere. It is more common in darker skinned Europeans or Middle-Eastern women. It causes a great deal of distress and onset may be at puberty.
Hirsutism is the result of the conversion of fine vellus hair to coarse terminal hair induced by androgens. These may be endogenous (adrenal, pituitary or ovarian origin) or exogenous (androgenic drugs). Excessive androgens will also result in virilism, amenorrhoea and infertility. Investigations should include:
However, end-organ sensitivity in idiopathic hirsutism is more common, in which investigations indicate hormone status to be normal.

Idiopathic hirsutism
Physical methods of hair removal include:
Medical treatment may be helpful: spironolactone, ethinyloestrodiol/cyproterone contraceptive pill or 50-200mg cyproterone for days 1 to 10 of the menstrual cycle.
Hypertrichosis may be congenital (hairy congenital naevi, hypertrichosis lanuginose and familial hypertrichosis) or acquired. Acquired hypertrichosis may be due to medications (ciclosporin, minoxidil, antiepileptics) or disease (hypercorticism, hypothyroidism, porphyria cutanea tarda, anorexia nervosa). Medical treatment should be directed at the underlying disease.

Congenital hypertrichosis

Becker naevus

Effect of ciclosporin
Discuss the psychosocial impact of hair loss in adolescents
Information for patients
See the DermNet bookstore