Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Nonmelanocytic congenital naevi
Created 2008.
Learning objectives
- Describe clinical features and management of non-melanocytic congenital naevi
Introduction
Naevi are benign proliferations of cells within the tissue of origin. They may be congenital (birthmarks) or acquired.
Congenital naevi consist of clusters of epidermal or dermal cells with numerous clinical variants. Melanocytic naevi have been described in the previous section. Other epithelial naevi include epidermal naevi and follicular naevi. Dermal naevi may be vascular or composed of connective tissue elements. There are also naevi derived from subcutaneous fat.
Epidermal naevi
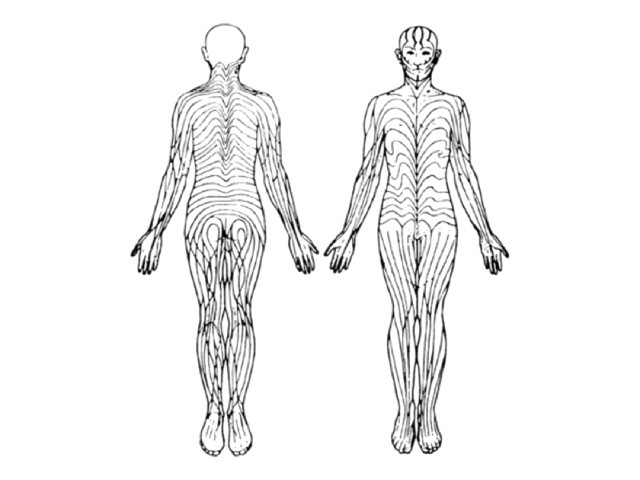
Epidermal naevi are ectodermal in origin and primarily composed of keratinocytes. Although often present at birth, 50% develop during the first year. They are thought to arise from mosaicism, i.e. a population of cells derived from one parent with point mutations in keratin genes. Epidermal naevi are distributed along the lines of Blashko.
Lines of Blaschko Lines of Blaschko 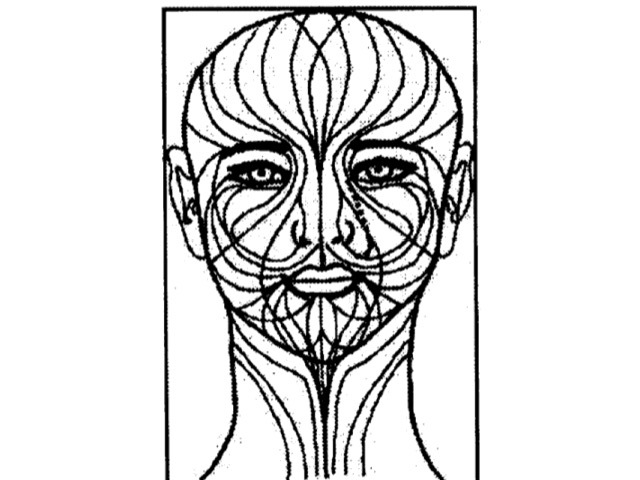
Linear epidermal naevus
Unilateral, skin coloured or brown warty plaque or plaques on the trunk and/or limbs. They tend to become more extensive and thickened with age.
Systematised epidermal naevus
Multiple swirling lesions on one or both sides of the body associated with skeletal and central nervous system abnormalities.
Epidermal naevus Epidermal naevus Epidermal naevus 


Other characteristic subtypes include epidermolytic epidermal naevus, acantholytic epidermal naevus and linear porokeratosis.
Linear porokeratosis 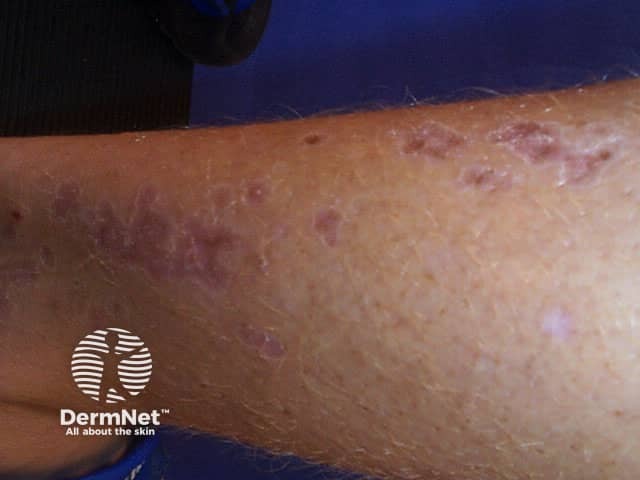
Epidermal naevus syndromes
The epidermal naevus syndromes refer to the association of an epidermal naevus with abnormalities in other organ systems derived from the embryonic ectoderm. These syndromes may involve the eyes, bones or nervous system. Many specific syndromes have been described including CHILD syndrome and Proteus syndrome.
Organoid naevi
If appendageal structures are included, the term organoid naevus may be used. There are several distinct types.
Becker naevus
This mainly affects males with onset at puberty, presumably stimulated by circulating androgen. There is a large unilateral area of pigmentation, hypertrichosis and sometimes acne on the upper trunk or shoulder. It is sometimes associated with other ectodermal abnormalities.
Becker naevus Becker naevus Becker naevus 


Inflammatory linear verrucous epidermal naevus (ILVEN)
ILVEN is an epidermal naevus with inflammatory characteristics and can look similar to eczema or psoriasis. It can be extremely pruritic.
ILVEN 
Sebaceous naevus
The sebaceous naevus arises on scalp or face. A flat hairless oval patch at birth, it becomes more prominent and papillomatous at puberty. Various benign and malignant secondary tumours may arise within the naevus, so excision in early adult life is generally recommended. The sebaceous naevus syndrome is an association with other ectodermal abnormalitites.
Sebaceous naevi Sebaceous naevi Sebaceous naevi 


Comedone naevus
The comedone naevus is due to hair follicle proliferation; the follicles are plugged by keratin. The lesions are present at birth in both males and females and may be single or multiple. Occasionally they are associated with other ectodermal abnormalitites.
Comedonal naevus 
Naevi derived from sweat glands are uncommon.
Vascular naevi
Vascular naevi may be proliferative haemangiomas, which usually resolve, or vascular malformations including capillary, venous, and lymphangatic types. Mixed lesions occur.
Haemangioma
Haemangiomas are due to proliferating endothelial cells. They arise in 10% of neonates (especially premature), mostly on the head and neck area, grow for a year or so and then involute over the next 3 to 10 years. Capillary angiomas (strawberry naevus) are superficial lesions, cavernous angiomas are subcutaneous, and mixed types may be seen. Lesions growing over the eye, nose, mouth or genitals can cause functional problems and may require treatment (oral propranolol, laser therapy, endovascular ablation).
Superficial infantile haemangioma Deep infantile haemangioma Mixed infantile haemangioma 


Rapidly growing cavernous haemangioma may rarely result in heart failure.
Capillary malformations
Capillary malformations are telangiectatic and include salmon patch (affecting the nape of the neck, forehead or eyelid of 40% neonates) and port wine stain (0.3% neonates). The salmon patch tends to fade or disappear, but port wine stains become more prominent in adult life. Commonly on the face and neck, they may have severe psychosocial impact. Capillary vascular naevi may be associated with other malformations in Sturge-Weber (trigeminal origin), Parkes Weber (arteriovenous), Klippel-Trénaunay (hemihypertrophy) and Proteus (multiple abnormalities) syndromes.
Salmon patch (stork mark) Infantile port wine stain Adult port wine stain 


Angioma serpiginosum
Angioma serpiginosum appears to be a late-onset naevoid vascular disorder. It presents during childhood as clusters of red puncta in a linear, serpiginous or gyrate pattern.
Angioma serpiginosum 
Venous malformations
Venous malformations can be identified by blue superficial lesions or present with deeper swelling. Types include glomuvenous malformations, arteriovenous malformations and blue rubber bleb naevus syndrome.
Blue rubber bleb naevi 
Lymphatic malformations
These were misnamed ‘lymphangioma’ but are not proliferative. They include the large cystic hygroma, deeply seated cavernous lymphangioma and the superficial, microcytic lymphangioma circumscription. Plaques or solitary papules may be skin coloured, red, blue or brown and superficial lesions appear similar to frogspawn.
Cystic hygroma Cavernous lymphangioma Lymphangioma circumscriptum 


Connective tissue naevi
Connective tissue naevi are uncommon. They are sometimes found in other diseases including tuberous sclerosis, proteus syndrome and congenital syphilis. Types of connective tissue naevus include:
- Collagenoma
- Elastoma
- Congenital smooth muscle hamartoma
- Fat naevus
- Congenital fibromatosis (infantile myofibromatosis)
- Mucinous naevus
Collagenoma Collagenoma (shagreen patch) Elastosis perforans serpiginosa 


Elastosis perforans serpiginosa presents in adolescence with extrusion of abnormal elastic fibres through the epidermis. Groups of scaly papules are generally arranged in an arc or ring shape on the neck or forearms. EPS is associated with other disorders of connective tissue such as Marfan syndrome, Ehlers Danlos syndrome, osteogenesis imperfecta, pseudoxanthoma elasticum and Down syndrome.
Activity
What information about treatment can you give the parents of a child with a facial port wine stain? What are the requirements to obtain District Health Board funding for treatment?
References:
On DermNet:
Information for patients
Other websites:
- Medscape Reference: Benign neoplasms
Books about skin diseases:
See the DermNet bookstore
