Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
Dermatology is the branch of medicine that deals with skin, mucous membranes, hair and nails. Although relatively straightforward to examine, the skin is the largest organ and has numerous potential abnormalities - there are about 1500 distinct skin diseases and many variants. We are relatively ignorant about the pathogenesis of the majority of these although knowledge is rapidly increasing especially in the fields of molecular medicine and genetics.
This course will discuss the impact of skin diseases, outline the biology of normal skin, and describe how to examine the skin and how its diseases may be effectively treated. A range of skin infections, inflammatory skin diseases and neoplastic conditions will be briefly described.
UK data suggests an average of 15% of consultations in general practice relate to a skin problem and between 50 and 75% of individuals may have a skin problem at any time. Although most of these are relatively harmless and asymptomatic, (warts, athletes' foot, dandruff, insect bites and so on), many result in significant disability.
Symptoms of skin disease include:
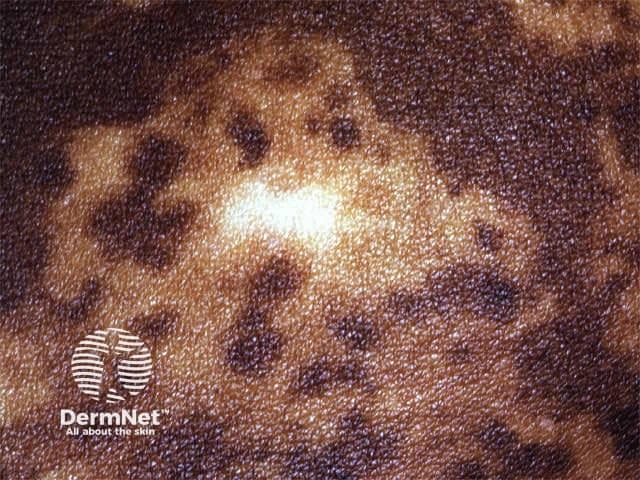
Signs may be described in terms of single areas of altered skin (lesions) or widespread eruptions. The distribution, configuration, colour, morphology, surface and secondary changes may be helpful in making a diagnosis and planning management.
Skin diseases are classified in various ways.
However, these classifications are evolving as the science of dermatology expands. The importance of genetic predisposition and immune function are increasingly recognised.
Reed codes, DRGs and the International Classification of Diseases (ICD-10) are not adequate for dermatological diagnoses.
There have been various attempts to name and categorise skin diseases and these are evolving. Confusion in terminology has resulted in several names for the same disorder, and several different disorders have been given the same name. The British Association of Dermatologists (BAD) Index is a comprehensive list, with subclasses allowing up to six figures/letters for precision. There is overlap where a specific condition may be assigned more than one code.
A. Infectious diseases affecting the skin
B. Reactions to mechanical, thermal, cold and radiation stimuli
C. Dermatitis/eczema and related conditions
D. Psoriasis and other acquired keratinising disorders
E. Papulosquamous and granulomatous disorders of the skin
F. Urticarias, erythemas and other inflammatory dermatoses
G. Disorders of skin colour
H. Disorders of skin appendages
J. Disorders involving cutaneous vasculature
K. Disorders of the dermis and subcutaneous tissue
L. Site-specific dermatoses
M. Connective tissue, immunobullous and related diseases
N. Metabolic and nutritional disorders affecting the skin
P. Psychological, psychiatric and neurological disorders affecting the skin
Q. Cutaneous markers of internal disorders
R. Dermatoses resulting from treatment or from poisons
S. Genetic and chromosomal disorders affecting the skin
T. Dermatoses specific to age or sex
W. Naevi, hamartomata and developmental anomalies of the skin
X. Neoplasias, tumours and cysts of the skin and appendages
Y. Benign and malignant infiltrations of the skin
Z. Diagnosis not coded
An online database of dermatological terminology, DermLex the Dermatology Lexicon, is now accessible on the American Academy of Dermatology's website (September 2009).
Certain skin problems may be more prevalent in specific populations.
| What conditions do you think white-skinned New Zealanders are particularly prone to? |
White-skinned New Zealanders are particularly prone to conditions relating to excessive exposure to ultraviolet radiation in skin that has inadequate natural protection. These include photoageing changes (e.g.. dryness, freckling, fine wrinkles) and malignancies (e.g. actinic keratoses, basal and squamous cell carcinoma, melanoma).
Old skin 
Black skin is particularly prone to pigmentary disorders and hypertrophic or keloidal scarring.
Skin diseases prevalent in the tropics often have infectious origins.


Occupational dermatological diseases often relate to the irritant nature of material with which workers are in contact and sometimes to immune reactions to specific allergens. Hand dermatitis is the most common occupational skin problem. Examples:
Hand dermatitis Hand dermatitis 

| What are the the occupational and social impacts of the conditions illustrated below? |
Vitiligo Penile psoriasis Haemangioma 



Most dermatological conditions are highly visible and may invoke disgust, shame and self-consciousness that can have profound psychosocial effects. Disfigurement can result in negative self perception, depression, social rejection and social isolation related to unfavourable self-image. Emotional abuse, verbal abuse and bullying may take place. These in turn can lead to self-contempt, frustration and torment leading to deliberate self harm or even suicide (a recognised complication of disfiguring skin conditions such as acne).
In addition, psychiatric disorders may manifest as apparent skin disease. Therefore the management of skin diseases requires recognition of psychological aspects as well as treating the affected skin.
Outline pharmacological, cognitive and behavioural management of body dysmorphic syndrome
Information for patients
See the DermNet bookstore