Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2009.
Many skin diseases include the term ‘lichen’, which is thought to originate from a resemblance to the lichen that is found on trees.
Lichen simplex is a type of eczema and was discussed in the dermatitis section of this course. There are several other uncommon “lichen” conditions that will not be considered in this course.
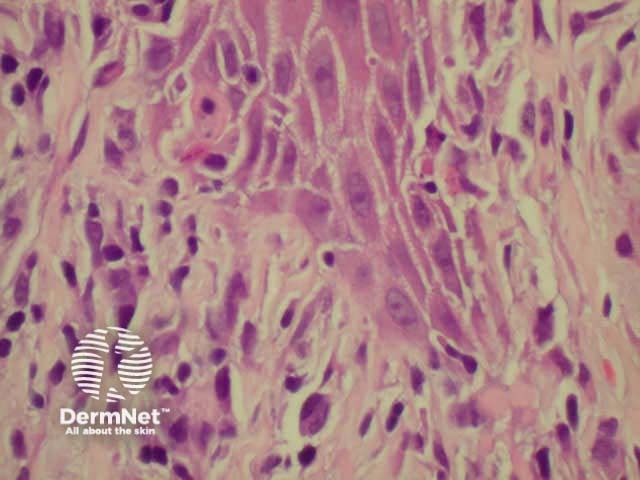
Lichenoid histology refers to liquefaction degeneration of basal layer, dermal infiltration of inflammatory cells hugging the basal layer, colloid bodies (degenerating keratinocytes) and dermal melanin.
Low power view Liquefaction degeneration 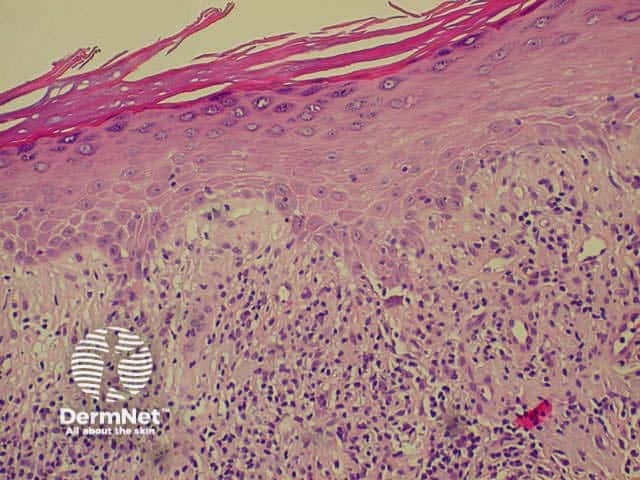
Idiopathic lichen planus has the following features:
Follicular lichen planus (lichen planopilaris) results in perifollicular erythema and scaling in the scalp and other hair bearing areas. It may or may not arise in association with non-follicular or mucosal disease.

The ventral wrist is a typical site

The shins is a common site

Hypertrophic lichen planus

Lacy-pattern in buccal mucosa

Nail dystrophy

Polygonal papules and plaques.
Treatment of lichen planus may include:
Erosive lichen planus affects the oral and/or genital mucosa. It may result in very painful ulceration and scarring.

Lichen planus

Lichen planus

Lichen planus
Lichenoid drug eruption has similar histology, and sometimes clinical appearance. More often there is a diffuse eruption of mildly irritable flat dry patches on trunk and limbs. Common causes include thiazides, anti-malarials, gold and ACE inhibitors.
Chronic graft-versus-host disease (GVHD) also has lichenoid histology. Arising more than 100 days after bone marrow transplantation, there are lichen planus-like papules and dermal sclerosis.
Lichen sclerosus is a common cause of vulval itching and soreness in menopausal women. Only ten percent of cases affect other sites or men. It is thought to have an autoimmune origin, with an extracellular matrix protein as antigen. On the vulva, perineum and perianal mucosa, it causes white plaques, atrophy, sclerosis (scarring), haemorrhage, blistering and ulceration. In children, it is often confused with the results of sexual abuse.

Axillary lichen sclerosus

Penile lichen sclerosus

Vulval lichen sclerosus

Extensive vulval, perineal

Hypertrophic lichen sclerosus

Perianal squamous cell carcinoma
Patients with lichen sclerosus should be under the care of a dermatologist. Ultrapotent topical steroids are generally successful but should be used with caution because of potential adverse effects.
Ichthyosis refers to a group of disorders of keratinisation characterised by excessively dry and scaly skin (abnormal differentiation and desquamation of the epidermis). Genetic analysis is identifying the protein abnormality responsible in specific subtypes.
The most common types of ichthyosis are:
Autosomal dominant ichthyosis vulgaris
Autosomal recessive lamellar ichthyosis
X-linked recessive ichthyosis
Bullous ichthyosiform erythroderma
Acquired ichthyosis is the dry skin associated with cachexia and certain forms of cancer and lymphoma. It is also characteristic in heavy consumers of kava.

Ichthyosis vulgaris

X-linked ichthyosis

Hyperlinear palms in ichthyosis vulgaris

Bullous ichthyosiform erythroderma

Bullous ichthyosiform erythroderma

Acquired ichthyosis in kava drinker
Treatment of ichthyosis requires regular application of emollients containing urea and/or lactic acid and the use of soap substitutes when bathing. Oral retinoids may be prescribed for severe cases.
Keratosis pilaris affects up to 50% of adolescents and may present from neonate to middle-age.

Keratosis rubra pilaris

Keratosis pilaris faciei

Follicular plugging
Keratosis pilaris rarely clears with treatment. Urea-containing emollients may soften the affected areas. Topical retinoids encourage normal follicular keratinisation with improvement in the appearance in some patients but may irritate.
Pityriasis rubra pilaris (PRP) is the name given to a group of rare skin disorders resulting in localised erythematous scaly plaques rather like psoriasis. However there is less scaling and prominent follicular involvement. Keratoderma of palms and soles is usual. Both juvenile and adult types may result in erythroderma.

Juvenile PRP

Palmar keratoderma

Follicular papules
An uncommon inherited disorder with disordered keratinisation, resulting in characteristic greasy reddish papules in scalp and trunk, palmar pitting and nail changes. The onset of skin lesions is generally during adolescence. Darier disease may be complicated by sunburn, staphylococcal infection, and herpes simplex virus infection

Darier disease

Darier disease

Darier disease

Darier disease

Darier disease

Darier disease
Darier histology has the following features:
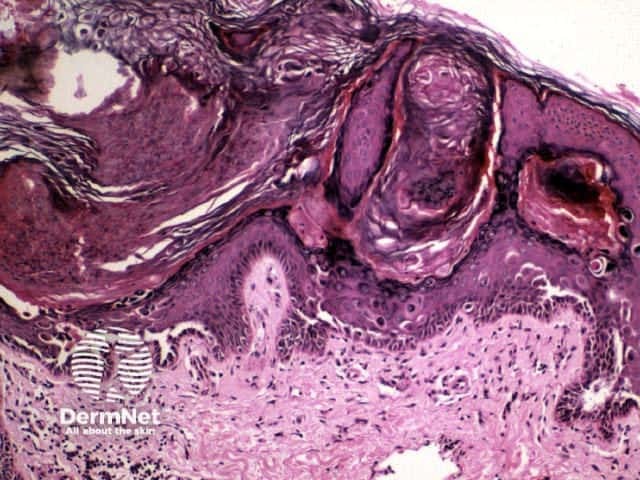
Low power view
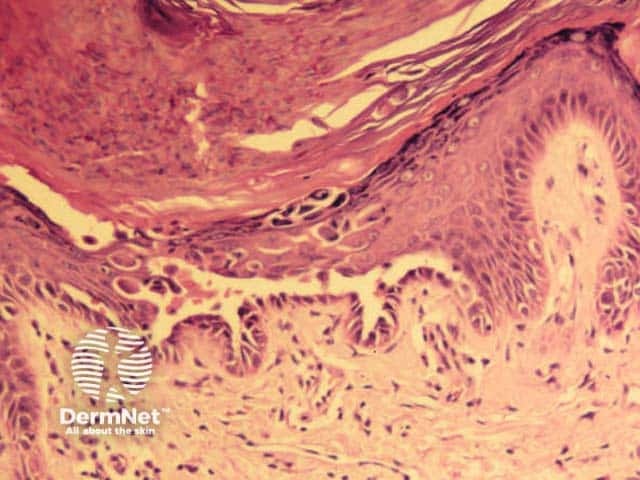
Close-up
Review the molecular genetics of keratin disorders.
Information for patients
See the DermNet bookstore