Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Topical therapy for psoriasis
Created 2009.
Learning objectives
- Prescribe topical therapy for psoriasis safely and appropriately
Introduction
Most patients with psoriasis use topical treatment of one form or other. As with all topical treatments, a range of products may be required depending on the site, severity and chronicity of the skin disease.
Keratolytics and emollients
Emollients relieve dryness, fissuring and irritation. Thick ointments based on white soft paraffin, beeswax or lanolin are recommended for chronic plaques especially on hands and feet. Keratolytics such as salicylic acid (0.5%-10%) and/or urea (5-40%) reduce scaling and may be incorporated in shampoos, lotions, creams, ointments and pastes. Salicylism is a potential risk of extensive use of high concentration topical salicylic acid. Both salicylic acid and urea may irritate and cause transient stinging especially if the treated skin is fissured, excoriated or eroded.
Calcipotriol
Calcipotriol is a derivative of calcitriol (1,25-dihydroxy cholecalciferol or active vitamin D). Calcipotriol is available as an ointment, cream and scalp solution at a concentration of 50µg/g. It is mainly used to treat psoriasis plaques but may also be useful in other scaling conditions such as ichthyosis and epidermal naevi. It is applied twice daily to reduce scaling and induration. Erythema often persists despite continued treatment.
Topical calcipotriol is generally well tolerated, but sometimes causes stinging and/or irritant dermatitis, especially on the face. It appears to be safe long term but because of lack of safety data, it should be used with caution in children, during pregnancy or lactation.
Calcipotriol is inactivated by salicylic acid. If more than one 100g-tube is used each week in an adult, calcium levels in blood and urine should be monitored. Calcipotriol is very poisonous to dogs.
Daivonex® ointment contains calcipotriol Psoriasis prior to calcipotriol ointment Psoriasis after 6 weeks’ calcipotriol ointment applied twice daily 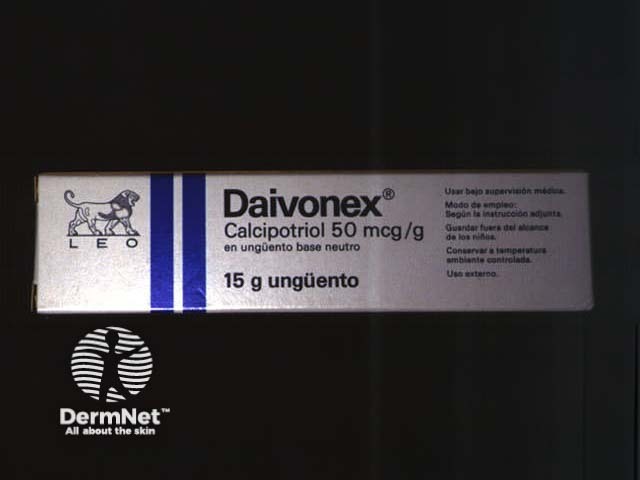


Topical corticosteroids
Topical corticosteroids are popular with patients because they are clean, well tolerated and easy to apply. However, they are not ideal long term because of tachyphylaxis and adverse effects. Potent or ultrapotent topical steroids may significantly improve the appearance of psoriasis, but they do not result in remission. They may be usefully combined with other topical agents including calcipotriol, salicyclic acid, antifungal agents.
A two to four-week course of ultrapotent steroid ointment will quickly improve the appearance of plaques on trunk and limbs (or solution for scalp disease). Its effect is enhanced by occlusion using adherent dressings or cling-film wrapped around the affected area. Ultrapotent topical steroids should be limited to short-term use.
- Weekend ‘pulse’ treatment with potent topical steroids may be suitable long term.
- Mild topical steroids in cream or lotion can be used for widespread disease or to relieve irritation
- Moderate potency topical steroid can be used as courses and / or weekend pulses for face, flexures and genital psoriasis
Steroid atrophy 
The patient illustrated has psoriasis. He has been applying clobetasol propionate ointment (an ultrapotent topical steroid) and has used about 100g each week for several months. He is also taking oral prednisone because of severe psoriatic arthropathy. He has developed severe striae and marked generalised cutaneous atrophy. Note the transparency of abdominal skin and Cushingoid habitus. His psoriasis was subsequently extremely difficult to control and he suffered several serious complications of steroid therapy.
Coal tar
Coal tar continues to be prescribed for patients with psoriasis and eczema. It is anti-inflammatory i.e. it reduces redness and itching. Pine tar and ichthammol preparations are also available.
Hospitalised patients with chronic plaque psoriasis may be prescribed 2-5% crude coal tar in an emollient base under dressings, preceded by daily exposure to ultraviolet radiation (Goeckerman regime). Crude coal tar is black, malodorous, messy and rarely used nowadays.
Crude coal tar ointment applied in Goeckerman regime Crude coal tar ointment applied in Goeckerman regime 

There are several over-the-counter and prescription products containing more cosmetically acceptable refined or liquified coal tar (liquor picis carbonis), often combined with salicylic acid as a descaling agent and/or sulphur, resorcinol and other traditional anti-inflammatory agents. They are most useful for scalp psoriasis and seborrhoeic dermatitis, applied for an hour or more before washing out with a shampoo also containing tar and salicylic acid.
Dithranol
Dithranol, also known as anthralin, is one of the most effective preparations available for treating psoriasis. It is not used for another skin conditions. The Ingram regime involves applying dithranol twice daily in Lassar’s paste (zinc, salicylic acid and paraffin) under tube gauze dressings. It may be preceded by a tar bath and exposure to ultraviolet radiation. This treatment method is really only suitable for inpatients and is rarely used nowadays.
Dithranol causes severe irritation on normal skin and stains skin and clothing a purple-brown colour. It wears off the skin within about ten days but leaves permanent marks on fabric. For outpatients, dithranol in a cream base is left on the skin for only 10 to 30 minutes. This ‘short contact’ method reduces burning and staining.
Dithranol stains 
Other topical agents
Other topical agents sometimes used for psoriasis may include:
- Topical calcineurin inhibitors (pimecrolimus and tacrolimus, which is not available in New Zealand in 2005). These are particularly useful for psoriasis in thin skinned areas i.e. face, genitals and skin folds
- Topical retinoids (e.g. tazarotene, not available in New Zealand in 2005); these are usually combined with other agents because of irritation.
Activity
Find out which preparations for psoriasis are currently subsidised by PHARMAC.
References:
On DermNet:
Information for patients
Other websites:
- Medscape: Quality of Life Considerations in Psoriasis Treatment from Dermatology Nursing 2003 Treating Psoriasis: The Dermatologist's Perspective CME presentation July 2005
Books about skin diseases:
See the DermNet bookstore
