Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Cutaneous medicine
Created 2009.
Learning objectives
- Recognise skin conditions that may be signs of endocrine, gastrointestinal, haematological and nutritional diseases
Introduction
Cutaneous signs can be a clue to the diagnosis of systemic diseases or may be a complication of them requiring specific attention. More details on specific skin conditions can be found in other parts of the course or On DermNet.
Endocrine disorders
Diabetes mellitus
- Diabetics have an increased risk of fungal and bacterial skin infections and the complications of arteriosclerosis, diabetic vasculopathy and neuropathy.
- About 50-80% of patients presenting with necrobiosis lipoidica have diabetes mellitus, most often Type 1.
- There is an association with granuloma annulare especially when generalised.
Necrobiosis lipoidica Close-up of necrobiosis lipoidica Granuloma annulare 


Thyroid disease
- Hypothyroidism may present with diffuse hair loss, dry skin and itching.
- Hyperthyroidism may also cause hair loss and itching, and pretibial myxoedema suggests Graves disease.
Pretibial myxoedema ‘Pretibial’ myxoedema on toe Eczema due to dry skin and hypothyroidism 

Cushing’s syndrome
Hypercorticism can result in acne, striae and cutaneous atrophy.
Moon face Striae due to systemic steroids 

Acromegaly
Growth hormone excess results in soft tissue hypertrophy, skin tags and seborrhoea.
Skin tags 
Addison’s disease
Lack of cortisol increases ACTH with resultant generalised hyperpigmentation.
Gastrointestinal disease
- Gluten sensitive enteropathy can be found in nearly all patients presenting with dermatitis herpetiformis.
- Malabsorption of zinc results in acrodermatitis enteropathica.
- Inflammatory bowel disease is associated with pyoderma gangrenosum, granulomatous cheilitis and pyodermatitis-pyostomatitis vegetans.
Dermatitis herpetiformis Pyoderma gangrenosum Gardner syndrome 


- Peutz Jeghers syndrome (lentigines on and around the lips) is associated with benign polyposis of the small bowel.
- Gardner’s syndrome (epidermal cysts and lipomas) is associated with large bowel polyps, which have a strong risk of malignancy.
- Birt-Hogg-Dubé syndrome (facial fibrofolliculomas) is associated with pneumothorax, renal and ovarian cancers.
Renal disease
Chronic renal failure is associated with:
- Pruritus
- Nodular prurigo
- Calcinosis and calciphylaxis (calcium deposition resulting in progressive cutaneous necrosis)
- Perforating collagenosis
- Porphyria cutanea tarda (see below) and pseudoporphyria (PCT-like rash but normal porphyrin biochemistry results).
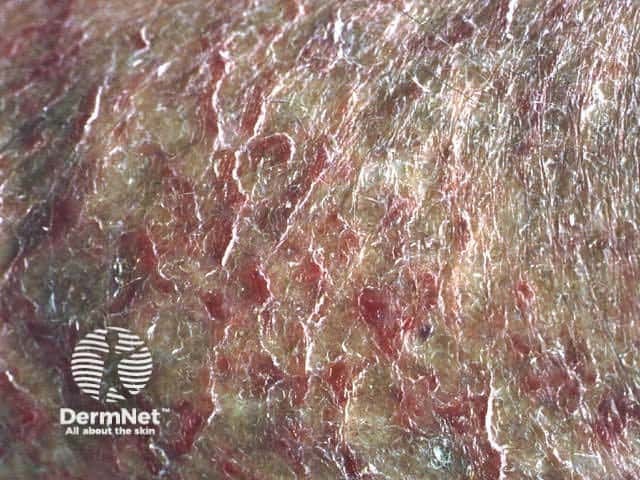
Calciphylaxis Renal pruritus Warts, actinic keratoses and squamous cell carcinomas 


Renal transplantation and the use of immunosuppressive medication gives rise to a high risk of viral infections (mainly warts) and skin cancers (especially squamous cell carcinomas). These may be very aggressive.
Haematological diseases
- Cutaneous haemorrhages (ecchymoses and petechiae) may be due to thrombocytopaenic purpura, disseminated intravascular coagulation (DIC) and cryoglobulinaemia.
- Generalised pruritus can be due to iron deficiency anaemia or polycythaemia rubra vera.
- Leukaemia may be associated with pyoderma gangrenosum and Sweet’s disease (acute neutrophilic dermatosis).
- Leukaemia / lymphoma sometimes causes erythematous, purpuric or ulcerated cutaneous nodules.
Porphyria
Porphyrias are due to abnormalities of the haem pathway and result in cutaneous photosensitivity. Diagnosis is confirmed by detection of excessive porphyrins in blood, urine or faeces. The most common to present to dermatologists are:
- Erythropoeitic protoporphyria (EPP)
- Porphyria cutanea tarda (PCT)
- Variegate porphyria (VP)
Erythropoeitic protoporphyria Urine of patient with porphyria cutanea tarda Hands in variegate porphyria 


- EPP presents in childhood with pain and blistering on minimal sun exposure.
- PCT and VP present with skin fragility, sub-epidermal bullae and hypertrichosis.
- PCT is associated with liver disease, hepatitis C infection, haemochromatosis, and excess alcohol or oestrogen ingestion.
- VP is associated with gastrointestinal porphyric crises and certain drugs may prove fatal.
Hyperlipidaemias
- Xanthelasmata are periorbital plaques containing cholesterol and may or may not be associated with hyperlipidaemia.
- Cutaneous eruptive, tuberous, plane or tendinous xanthomata are nearly always associated with specific patterns of primary or secondary hyperlipidaemia.
Xanthelasma Eruptive xanthomata Tuberous xanthoma 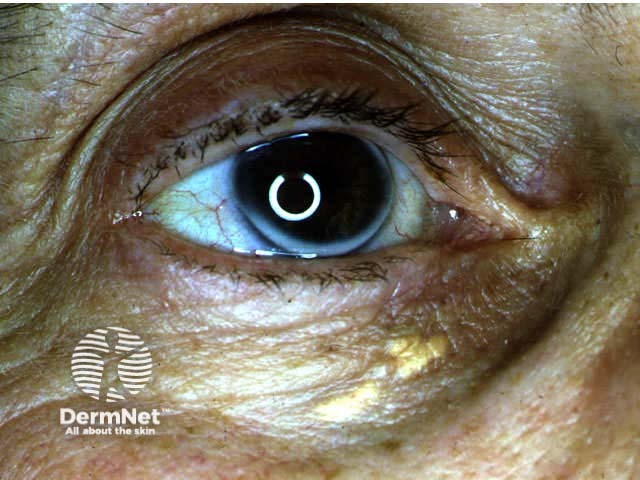


Behçet’s disease
- Behçet’s disease (rare in New Zealand) may cause oral and genital ulceration, pustules and erythema nodosum.
- Patients may also have iritis, arthritis, gastrointestinal ulceration and neurological problems.
- Pathergy refers to the development of pustules and / or ulceration following needle injury.
Vulval ulceration Pathergy 

Nutritional disorders
Scurvy
Vitamin C deficiency presents with corkscrew hairs and bleeding gums or easy bruising and may occur in the elderly. Low levels of leucocyte ascorbic acid confirm the diagnosis.
Pellagra
Nicotinic acid deficiency presents with photosensitive eruption on neck and feet, diarrhoea and dementia.
Kwashiorkor
Protein deficiency may cause dry red skin and hair and is associated with oedema and ascites.
Fatty acid deficiency
Fatty acid deficiency in infants or with total parenteral nutrition may result in dry red skin and delayed healing.
Obesity
- Bacterial and fungal infections especially in skin folds (intertrigo)
- Skin tags, acanthosis nigricans, striae
- Frictional trauma: intertrigo, irritant dermatitis, Koebnerised psoriasis
- Hyperhidrosis and bromhidrosis (offensive body odour).
Pellagra
Pellagra Pellagra Pellagra 


Amyloidosis
- Amyloidosis is an extracellular deposition in various tissues of amyloid fibril proteins.
- Systemic primary amyloidosis occurs in patients with plasma cell dyscrasias and multiple myeloma. Skin signs include pinch purpura and waxy papules.
- Secondary amyloidosis follows chronic inflammatory disease and rarely causes skin signs.
- Localised cutaneous amyloidosis results in macules, papules, plaques and nodules.
Macroglossia Macular cutaneous amyloidosis 

Sarcoidosis
Sarcoidosis is diagnosed histologically by the presence of noncaseating granulomas in the skin, lymph nodes, lungs, liver, spleen, eyes, parotid glands or joints. The mainstay of treatment is systemic corticosteroids.
Cutaneous features are highly variable:
- Papules, nodules, plaques and ulcers may occur.
- These may be flesh-coloured, violaceous or brown characteristically with translucent hue.
- Lupus pernio affects nose, cheeks, ears and fingers and is associated with severe pulmonary disease.
- Erythema nodosum associated with bihilar lymphadenopathy is due to pulmonary sarcoidosis and has a good prognosis.
Scar sarcoidosis Facial granulomas Extensive plaques Lupus pernio Bihilar lymphadenopathy Erythema nodosum 





Acquired immunodeficiency syndrome
Acquired immunodeficiency syndrome (AIDS) is due to infection of T cells with human immunodeficiency virus (HIV) resulting in progressive immunodeficiency and a decrease in T-cell helper / suppressor ratio.
A variety of cutaneous inflammatory conditions, infections and malignancies arise and tend to be more vigorously expressed than in normal individuals.
Activity
How may xanthelasma be removed?
References
On DermNet
Information for patients
Other websites
- Emedicine: Internal medicine
