Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Selecting patients for teledermatology
Created 2017.
This course is designed to help general practitioners manage patients with skin cancer and to make appropriate referral to stretched specialist services.
Referral requires:
- Skin lesion history
- Background social medical history, drugs and allergies
- High quality images:
-
- Anatomic/location images
- Macroscopic/close-up images
- Dermatoscopic images
- Relevant histopathology results.
Inadequate information will lead to rejection of the referral, leading to delays in diagnosis/management and unnecessary expense.
Suitable patients may include:
- In New Zealand, residents entitled to District Health Board funding
- Any age, gender and ethnicity
- Insured and uninsured people
- People with limited access to specialist care due to age, infirmity, incarceration, institutionalisation, lack of time, geographic location etc.
Suitable lesions may include:
-
Typical skin cancers
These patients could instead be referred directly to a treatment service. However, many can be managed in general practice, and teledermatology advice regarding appropriate management can be helpful.
The teledermatologist can also suggest which expert service is appropriate.
-
Lesion of uncertain significance
If differential diagnosis includes melanoma and/or nonmelanoma skin cancer, expert opinion reduces unnecessary excision of benign lesions and enables early removal of skin cancers.
-
Benign skin lesions
Management advice might be sought.
Unsuitable patients/lesions may include:
-
Sun-damaged patients that require full skin examination.
General practitioners should insure that they have examined the patient fully and that they have the skills and knowledge to identify skin cancers. A teledermatology service is intended for single or few lesions of concern.
-
Asymptomatic, typical benign skin lesions
Faster cancer treatment programme
The New Zealand Ministry of Health has targeted 11 cancers to be included in its faster cancer treatment programme, including melanoma. Note that nonmelanoma skin cancers are not included in this pathway.
The intention is to achieve national consistency for melanoma care in the following areas:
- Prevention and early identification
- Timely access to services
- Communication and referral
- Data collection
- Investigation, diagnosis and staging
- Multidisciplinary care
- Supportive care
- Care co-ordination
- Treatment
- Follow-up and surveillance
- Clinical monitoring and research.
Note:
“The tumour standards are not mandatory. Over the coming years DHBs will be expected to work with their regional cancer network and other local service providers involved in cancer services to use the tumour standards to review existing services and make improvements.”
A definition for 'high suspicion of cancer' (HSCan, melanoma) has been published. It is intended that lesions referred to public hospital melanoma clinics with these criteria and accepted at triage as suspicious of invasive melanoma will receive First Specialist Assessment (FSA) appointment within 14 days. HSCan does not include confirmed melanoma, i.e., one that has histological diagnosis.
The provisional standards indicate that teledermatoscopy reports are received by the referrer within five working days of the examination being performed.
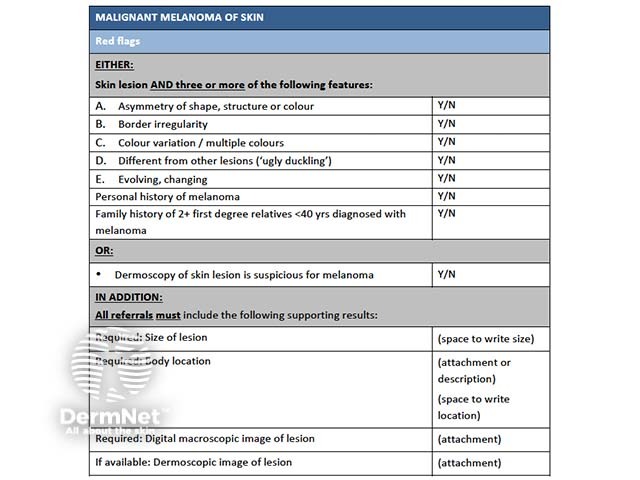
Criteria for melanoma
