Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lesions (benign) Diagnosis and testing
Author: Adjunct A/Prof Patrick Emanuel, Dermatopathologist, Clinica Ricardo Palma, Lima, Peru. DermNet Editor-in-chief: Adjunct A/Prof Amanda Oakley. Copy edited by Gus Mitchell. July 2018.
Introduction
Histology
Special studies
Differential diagnoses
Cutaneous plasmacytosis presents with multiple reddish-brown nodules. It has most often been reported to affect the trunk but is also known to affect the face and extremities in adults and is predominantly seen in Asians. The aetiology is poorly understood.
In cutaneous plasmacytosis, histopathological examination shows perivascular and perineural plasma cell infiltrates in the dermis (figures 1–4) without evidence of folliculitis or other common causes of plasma cell infiltrates (figures 1–4)
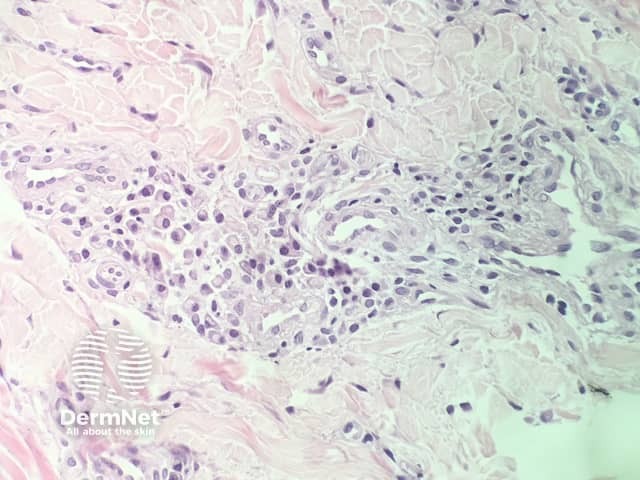
Figure 1
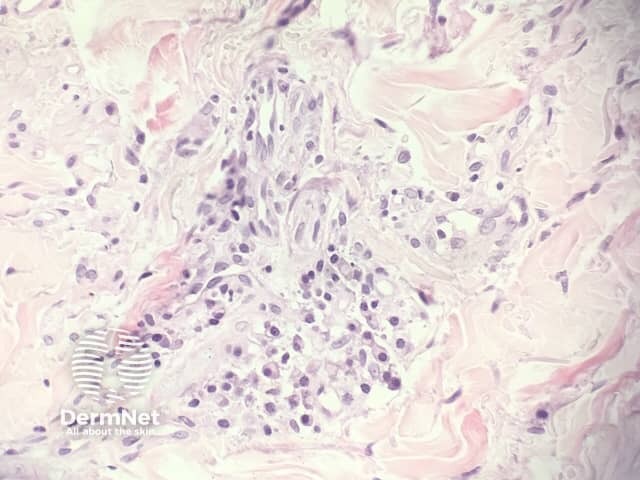
Figure 2
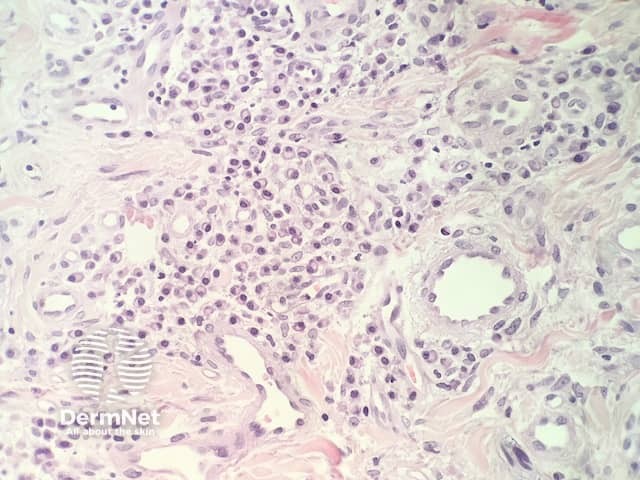
Figure 3
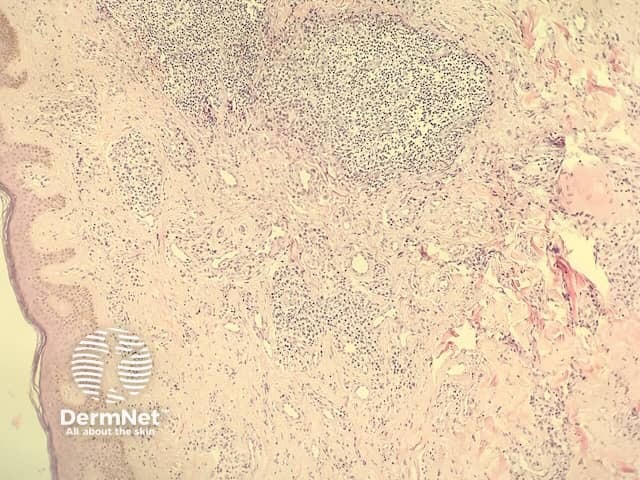
Figure 4
It is important to demonstrate that the plasma cells are polyclonal. This can be done with kappa and lambda immunohistochemistry or in situ hybridisation.
Other diagnoses to be considered include: