Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Immunoglobulin E tests — extra information
Immunoglobulin E tests
Author: Dr Tim Aung, Primary Care Practitioner, Brisbane & Logan, Queensland, Australia. Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. February 2019.
Immunoglobulin E (IgE)
Type I Hypersensitivity reaction
IgE test
Indications for IgE testing
Allergens tested
IgE level results
IgE level result interpretation
IgE testing vs. skin prick testing
What is immunoglobulin E?
Immunoglobulin E (IgE) is an antibody produced during a type I hypersensitivity reaction to an allergen. (See DermNet's page Allergies explained.) A schematic for the type I reaction pathway is shown below [1].
IgE antibodies are normally found in small amounts in the blood. A higher level than normal infers an allergic disorder may be present [2].
What is a type I hypersensitivity reaction?
Following exposure and re-exposure to an antigen (allergen) in susceptible individuals, a type I, or immediate, allergic reaction involves antigen-presenting cells, the activation of T-helper (Th) cells, the stimulation of B cells that release specific IgE, and the release of various pharmacological mediators (such as histamine, cytokines, leukotrienes, and others) from mast cells and basophils. The release of the mediators causes symptoms such as sneezing, wheezing, and weals.
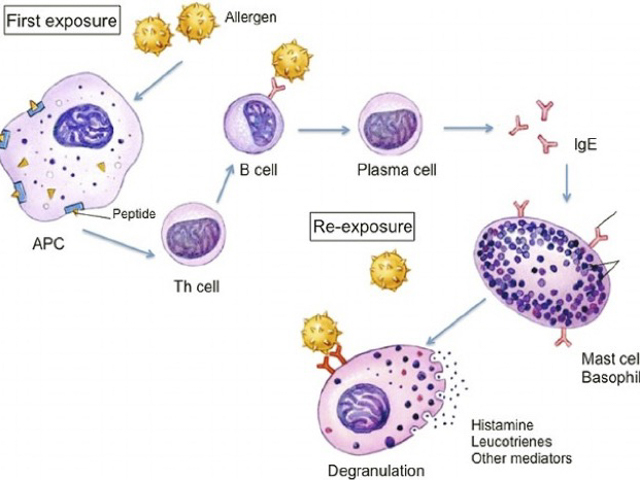
Type 1 hypersensitivity reaction
APC, antigen-presenting cell; IgE, immunoglobulin E; Th, T-helper [cell].
Credit: Gaurab Karki, Microbiologist Kathmandu, via Online Biology Notes.
What is an IgE test?
An IgE test is a blood test that detects circulating IgE. The test includes two types of test:
- Testing for total IgE — the total level of IgE in the blood.
- Testing for specific IgE — the level of specific IgE against a particular allergen.
Total IgE and specific IgE tests can be ordered at the same time or independently.
IgE levels can be measured using one of several methods. The use of the radioallergosorbent test (RAST) to measure IgE has been superseded by the use of enzyme-linked immunosorbent assays (ELISA), fluorescent enzyme immunoassays (FEIA), and chemiluminescent immunoassays (CLIA) [3,4].
Vacutainers

Removing blood for IgE tests
The colour of the top of the tube denotes what tests it is suitable for. In this case, the tube with the gold top (a serum separator tube) is used for IgE tests.
What are the indications for IgE testing?
An IgE test is indicated when the taking of a careful patient history and an examination lead to a suspicion of type I allergy.
An IgE test can also be used for monitoring a patient with a known allergic condition, such as:
- Anaphylaxis
- Allergic rhinitis (hay fever)
- Allergic conjunctivitis
- Asthma
- Chronic rhinosinusitis.
IgE tests are also useful to determine whether a patient is allergic to a specific protein, such as:
- Types of food allergy (eg, peanuts)
- House dust mites
- Grass, weed or tree pollens
- Animal dander or fur
- Certain drugs and cosmetics
- Moulds
- The venom of a bee or wasp.
An IgE test can be used when skin prick testing is not available or is unsuitable; for example, in an individual with dermographism, extensive skin disease, recent use of antihistamines or systemic steroids, or when there is concern that prick testing could cause an anaphylactic reaction.
IgE testing is rarely indicated in atopic dermatitis, allergic contact dermatitis, chronic spontaneous urticaria, or angioedema as the relevance of elevated IgE is uncertain in these diseases.
Choosing Wisely recommendations
Although there is no absolute contraindication for IgE tests, the American Academy of Allergy, Asthma & Immunology, the Australasian Society of Clinical Immunology and Allergy, and Choosing Wisely make the following recommendations [5,6].
- Don’t perform an indiscriminate battery of IgE tests in the evaluation of allergy.
- Food-specific IgE testing should not be performed without a clinical patient history that is suggestive of IgE-mediated food allergy.
- Specific IgE testing for inhalants or foods is not indicated in urticaria unless there is a clear history implicating an allergen as a provoking or perpetuating factor for the urticaria.
- Indiscriminate batteries of IgE tests for foods are expensive and not useful, potentially leading to erroneous diagnoses and inappropriately restrictive diets.
Which specific allergens can be tested?
The specific allergens that can be tested can be classified as follows [7]:
- Aeroallergens (inhalants)
- Indoor allergens — including house dust mites, animal dander (eg, cat, dog, and cockroach), mould, and fungal spores
- Outdoor allergens — such as pollens (from grasses, rye, weeds, and trees) and polluted air (smoke)
- Food allergens — including milk, eggs, peanuts, tree nuts, wheat, soy, codfish, and shellfish
- Venoms — including bee, wasp, hornet, ant venoms
- Dust mites (Dermatophagoides)
- Medicines — such as penicillin, aspirin, and others
- Latex
- Metals (especially nickel, cobalt, chromium, and zinc)
- Household chemicals
- Cosmetics.
IgE tests are also available to test different mixes of allergens. These include a:
- Food mix (ie, egg white, milk, codfish, wheat, peanut, and soybean)
- Cereal mix (ie, wheat, oat, corn, sesame seed, and buckwheat)
- Fruit mix (ie, banana, pear, peach, and apple)
- Seafood mix (ie, codfish, shrimp, mussel, tuna, salmon)
- Grass mix (ie, Bermuda, rye, Timothy, meadow, Johnson, and Bahia grasses)
- Tree mix (ie, olive, willow, eucalyptus, white pine, Melaleuca)
- Nut mix — routine (ie, peanut, hazelnut, brazil nut, almond, and coconut)
- Nut mix — extra (ie, pecan nut, cashew nut, pistachio, and walnut)
- Mould mix (ie, Penicillium, Aspergillus fumigatus, Cladosporium, Candida albicans, and Alternaria).
How are IgE levels reported?
The total IgE reference range depends on the age of the individual (it ranges from 0 to 4 kU/L in a newborn and 0 to ~148 kU/L in an older child or adult).
The result of a specific IgE test is reported for a grouped allergen mix or an individual allergen. The table below shows how the results are typically rated and interpreted [2,8,9].
Table. IgE level test ratings and interpretations
Rating of specific IgE level (kUA/L) |
Grade/Class |
Interpretation |
|---|---|---|
Absent or undetectable ( 0.35) |
0 |
Unlikely |
Low (0.35–0.69) |
I |
Doubtful significance |
Moderate (0.70–3.49) |
II |
Possible |
High (3.50–17.49) |
III |
More possible |
Very high (17.50–49.99) |
IV |
More likely |
Very high (50.00–100.00) |
V |
Very likely |
Extremely high (> 100.00) |
VI |
Extremely likely |
This table shows arbitrary international reference figures. The actual reference range and grading vary with the laboratory and are based on the method used for the test, calibration, the age of the patient, and the type of allergens.
How are IgE test results interpreted?
IgE test results should be carefully interpreted in the context of a patient’s presentation. High levels of total IgE can occur in allergic conditions, parasitic infections, certain immune-related disorders, and malignancies.
The sensitivity of specific IgE tests ranges from 60% to 95% and the specificity from 30% to 95%, depending upon the type of allergen and the age of the patient [3]. There is a good predictive value (> 90%) for food (cow’s milk, egg, fish, and peanuts), pollens (grass and trees) and dust mites. Tests for some medicines, latex, moulds, and venom have poor sensitivity but greater specificity [3,4]. Note:
- A positive test result means sensitisation to an allergen.
- The indicated level of IgE may not correlate with the extent or severity of symptoms when exposed to the allergen.
- A normal level of IgE may not exclude allergic disorders.
- A result may be misleading. False-positive and false-negative results can be due to cross-reactivity, the age of the patient, or the type and duration of exposure to the allergen.
Further evaluation can be done by skin prick testing or by challenging the patient to a specific allergen in vivo.
How does IgE testing compare with skin prick testing?
Skin prick testing is more specific than IgE testing and gives a rapid result (often within 30 minutes), but it requires a trained practitioner and is not always tolerated by young children.
Specific IgE blood tests are simple and safe. They can be expensive, depending on the number of allergens tested. Caution is required when interpreting the results [10].
References
- Karki G. Type I hypersensitivity reaction: mechanism and clinical manifestation. Available at: http://www.onlinebiologynotes.com/type-i-hypersensitivity-reaction-mechanism-and-clinical-manifestation/ (accessed 11 February 2019).
- Heyworth-Smith D, Campbell P. Laboratory Diagnosis of Allergy. QML pathology newsletter, Brisbane, 2017.
- Siles RI, Hsieh FH. Allergy blood testing: A practical guide for clinicians. Cleve Clin J Med 2011; 78: 585–92. doi: 10.3949/ccjm.78a.11023. PubMed
- Diaz RC, Liang J, Hallet L, Meyers AD. Diagnostic Allergy Testing: Specific IgE Testing. Updated February 29 2016. Medscape (accessed 7 Jun 2018).
- Don’t perform food IgE testing without a history consistent with potential IgE-mediated food allergy. Choosing Wisely. American Academy of Allergy, Asthma & Immunology. 3 March 2014. Available at: http://www.choosingwisely.org/clinician-lists/american-academy-allergy-asthma-immunology-food-ige-testing/ (accessed 5 February 2019).
- Food-specific IgE testing should not be performed without a clinical history suggestive of potential IgE-mediated food allergy. Australasian Society of Clinical Immunology and Allergy. Choosing Wisely. Available at: https://choosingwisely.org.nz/professional-resource/ascia/ (accessed 5 February 2019)
- Chapman MD. Allergen nomenclature. Clin Allergy Immunol 2008; 21: 47–58. PubMed
- Williams P, Sewell WA, Bunn C, Pumphrey R, Read G, Jolles S. Clinical immunology review series: an approach to the use of the immunology laboratory in the diagnosis of clinical allergy. Clin Exp Immunol 2008; 153: 10–8. doi: 10.1111/j.1365-2249.2008.03695.x. PubMed
- Sheldon J, Miller L. Allergy diagnosis reference guide. Clinical Biochemistry, East Kent University Hospitals, NHS. October 2014. P-6.
- Australasian Society of Clinical Immunology and Allergy (ASCIA). Laboratory Tests in the Diagnosis of Allergic Diseases. Updated January 2010. Available at: www.allergy.org.au/health-professionals/papers/tests-in-the-diagnosis-of-allergic-diseases (accessed 8 June 2018).
