Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Neurofibromatosis — extra information
Neurofibromatosis
Author: Vanessa Ngan, Staff Writer, 2003. Updated by Dr Ebtisam Elghblawi, Dermatologist, Tripoli, Libya. DermNet Editor in Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. October 2017.
What is neurofibromatosis?
Neurofibromatosis (NF) is a neurocutaneous genetic disorder that affects the bone, soft tissue, skin, and nervous system.
Multiple cutaneous neurofibromas


Neurofibromatosis

Neurofibromas
At least 8 different clinical phenotypes of NF have been identified. It is classified into 2 distinct types:
- Neurofibromatosis 1 (NF1)
- Neurofibromatosis 2 (NF2).
Neurofibromatosis 1
NF1 occurs in about 1 in 3000 births. It also known as von Recklinghausen disease. It is characterised by the presence of:
- 6 or more café-au-lait macules — flat light brown birthmarks
- Freckling in skin folds
- Lisch nodules in the iris of the eye.
- Multiple neurofibromas — tumours that hang off the skin
Neurofibromatosis 2
NF2 occurs in about 1 in 50,000 births. It also known as bilateral acoustic neurofibromatosis or central neurofibromatosis. It is characterised by multiple tumours and lesions on the brain and spinal cord.
Solitary neurofibroma is not associated with NF1 or NF2.
What causes neurofibromatosis?
NF1 and NF2 occur as a result of defects in different genes.
- NF1 is caused by a mutation on the neurofibromin gene located on the pericentromeric region of chromosome 17.
- NF2 is caused by a mutation on chromosome 22.
The mutated gene can be inherited from a parent who has NF by autosomal dominant transmission, or it can be a founder gene due to spontaneous mutation. A parent with NF has a 50% chance of passing the gene on to each of their children.
Genetics of Neurofibromatosis 1 and 2*
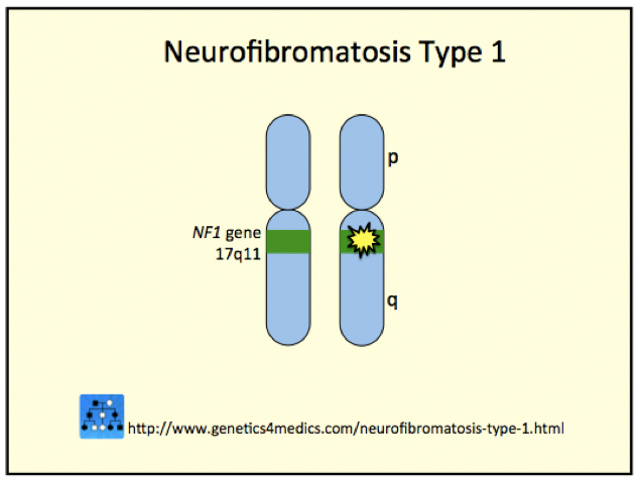
Neurofibromatosis Type 1
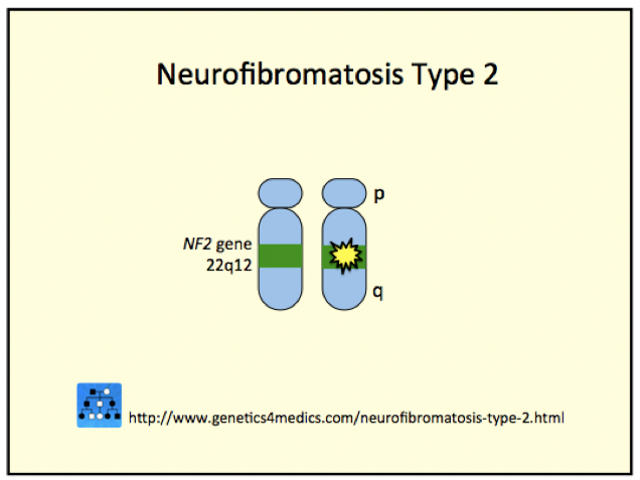
Neurofibromatosis Type 2
*Image courtesy Genetics 4 Medics
What are the clinical features of neurofibromatosis?
The extent and severity of manifestations of NF vary greatly from person to person and varies within the same family.
Neurofibromatosis 1
Café-au-lait macules
Café-au-lait macules are defined, oval or irregularly-shaped, light brown patches greater than 0.5 cm in diameter. They may be present at birth and increase in number during the first few years of life.
Although isolated café-au-lait macules can be found in many people without NF, individuals with more than 5 of these have a good chance of also having NF1, particularly if they appear on the skin within the first 5 years of life.
More than 5 café-au-lait macules are found in 1.8% of newborns, 25–40% of children, and 14% of adults with NF1.
Axillary freckling
Freckling in the armpits, known as Crowe sign, is characteristic of neurofibromatosis type 1. The freckles appear during puberty, after the development of café-au-lait macules and before neurofibromas. They may also appear in other skin folds such as the groin.
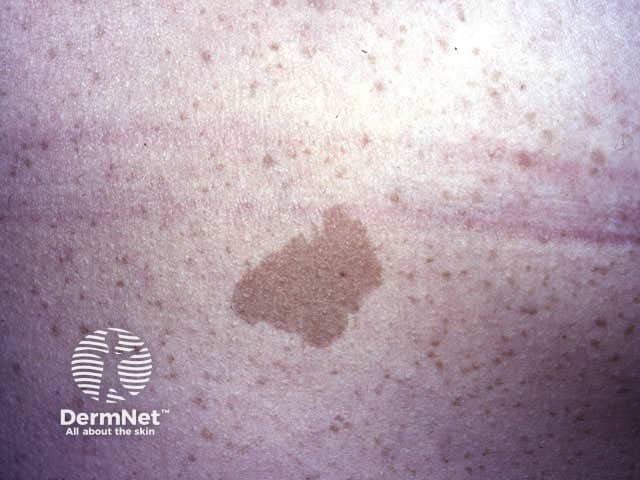
Café-au-lait macule

Café-au-lait macule

Freckling in the armpit
Lisch nodules
Lisch nodules are tiny tumours on the iris of the eye. After puberty, Lisch nodules are present in 97–100% of patients with NF1. Clinically, they do not cause any problems but help to confirm diagnosis.
Neurofibromas
Neurofibromas are composed of Schwann cells, fibroblasts, mast cells, and vascular components, and can develop at any point along a nerve. There are three types: cutaneous, subcutaneous, and plexiform. Cutaneous and subcutaneous neurofibromas are not specific for neurofibromatosis, but plexiform neurofibromas are only seen in NF1.
- Cutaneous neurofibromas are circumscribed, superficial, soft button-like brown, pink, or skin coloured superficial nodules with soft or firm consistency. They may demonstrate pathognomonic buttonhole invagination when pressed with a finger. They have no malignant potential.
- Subcutaneous neurofibromas are similar to cutaneous neurofibromas except deeper in origin. They may cause localised pain or tenderness.
- Plexiform neurofibromas present as bag-like masses within the skin. Nodular plexiform neurofibromas involve the dorsal nerve roots and diffuse plexiform neurofibromas are invasive tumours that may involve all layers of skin, muscle, bone, and blood vessels.

Neurofibroma

Neurofibroma

Plexiform neurofibroma
See more images of neurofibromatosis ...
Other features of NFI
The severity of cutaneous involvement in NF1 is not an indicator of the extent of the disease as internal manifestations are common and are often more serious. Problems in other parts of the body include:
- Malformation of the long bones (below the knee and elbow) and curvature of the spine (scoliosis)
- Short stature and growth hormone deficiency
- Learning difficulties, speech problems, and behavioural problems: 25–40% have learning disabilities, 5–10% may have intellectual disability
- Tumours on the optic nerve; these can cause loss of vision
- High blood pressure and other blood problems
- Tumours on the spine and brain; these increase risk of epilepsy
- Tumours or lesions on the gastrointestinal tract that may cause bleeding or obstruction
- Hearing defects.
Although most tumours are benign (non-cancerous), it is estimated that a person with NF1 has a 3–15% increased risk for developing cancerous tumours.
Neurofibromatosis 2
NF2 does not have as many outward signs as NF1. It is characterised by multiple tumours and lesions on the brain and spinal cord. The first symptom is usually hearing loss due to a tumour growing on one or both auditory nerves. Often this is not apparent until the late teens or early 20's.
Tumours in NF2 are usually benign. But benign tumour enlargement in the brain and spinal cord can interfere with vital functions.
Follow-up for patients with neurofibromatosis
The main role for follow-up is to monitor the development of tumours and intervene when necessary.
- Healthy children with NF should be followed-up and examined every 6–12 months by a paediatrician.
- Those with eye symptoms and signs should be assessed and monitored by an ophthalmologist.
- Hearing defects should be assessed and monitored by an otolaryngologist (ENT).
- A neurologist may need to examine the patient with any neurological symptoms and signs such as clumsiness, numbness or weakness.
Imaging with ultrasound scans, CT scans and MRI may be arranged to determine the site of any suspected tumour.
What treatment is available?
There is no cure for NF.
Neurofibromas that become large and painful can be cut out to reduce the risk of malignancy and other complications. Facial deformity can be mitigated by aesthetic (plastic) surgery.
Genetic counselling and education about NF is important. One concern that should not be overlooked is the risk of isolation or loneliness in people with NF. People with NF are often anxious about future complications and sometimes disfiguring lesions can lead to withdrawal from society.
Targeted molecular therapies show promise for the future treatment of neurofibromatosis. MEK inhibitors such as selumetinib may offer hope in reducing the size of plexiform neurofibromas and lighten cafe-au-lait macules.
Bibliography
- Farschtschi S, Mautner VF, McLean ACL, Schulz A, Friedrich RE, Rosahl SK. The neurofibromatoses. Dtsch Arztebl Int. 2020;117(20):354–60. doi:10.3238/arztebl.2020.0354 PubMed Central
- Ferner RE, Bakker A, Elgersma Y, et al. From process to progress-2017 International Conference on Neurofibromatosis 1, Neurofibromatosis 2 and Schwannomatosis. Am J Med Genet A. 2019;179(6):1098–106. doi:10.1002/ajmg.a.61112 PubMed Central
- Hom GL, Moodley S, Rothner AD, Moodley M. The clinical spectrum of mosaic neurofibromatosis in children and adolescents. J Child Neurol. 2020;35(3):242–6. doi:10.1177/0883073819889713 PubMed
- Tamura R. Current understanding of neurofibromatosis type 1, 2, and schwannomatosis. Int J Mol Sci. 2021;22(11):5850. doi:10.3390/ijms22115850 Journal
On DermNet
- Neurofibromatosis images
- Solitary neurofibroma
- Neurofibroma pathology
- Skin lesions, tumours and cancers
- Skin signs of neurological diseases
- Skin signs and systemic disease
Other websites
- Neurofibromatosis - OMIM – Online Mendelian Inheritance in Man
- Dermatologic Manifestations of Neurofibromatosis Type 1 – Medscape Reference
- Neurofibromatosis type 1 US National Library of Medicine Genetics Home Reference
- Children's Tumor Foundation
- The Neurofibromatosis Association
- Neurofibromatosis Association of New Zealand (email)
