Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Primary cutaneous anaplastic large-cell lymphoma — extra information
Primary cutaneous anaplastic large-cell lymphoma
Authors: Dr Germana Consuegra Romero, Dermatologist, Hospital Universitari General de Catalunya, Barcelona, Spain; Prof Pablo Fernández-Peñas, Dermatologist, Westmead Hospital, Sydney, Australia; Dr Jillian Wells, Dermatologist, Westmead Hospital, Sydney, Australia. Copy edited by Gus Mitchell. May 2021
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is primary cutaneous anaplastic large-cell lymphoma?
Primary cutaneous anaplastic large-cell lymphoma (pcALCL) is a rare type of indolent cutaneous T-cell lymphoma (CTCL) characterised by CD30+ atypical lymphocytes in the skin. It is classified as a primary cutaneous CD30+ lymphoproliferative disorder.


Who gets primary cutaneous anaplastic large-cell lymphoma?
Primary cutaneous anaplastic large-cell lymphoma can affect both sexes, all ages, and races. However, pcALCL affects males more often than females (3:1) and most cases are 50 to 70 years of age. Paediatric and congenital cases have been reported.
What causes primary cutaneous anaplastic large-cell lymphoma?
The aetiopathogenesis of primary cutaneous CD30+ lymphoproliferative disorders remains elusive. CD30 signalling affects growth and survival of lymphoid cells. Some studies suggest a restriction of the normal T-cell repertoire in the peripheral blood. Other hypotheses implicate reactive phenomena inducing CD30+ overexpression.
What are the clinical features of primary cutaneous anaplastic large-cell lymphoma?
- pcALCL usually presents as a rapidly-growing single nodule or plaque.
- The nodule is typically red to violaceous, at least 2 cm in diameter, and often ulcerates.
- Multiple localised grouped or generalised nodules occur in 20%.
- pcALCL lesions are usually asymptomatic.
- Any region of the skin can be affected, including mucosal surfaces. However, the upper half of the body is most commonly involved.
- Patients are systemically well with no fever, weight loss, or night sweats.



Dermoscopy of primary cutaneous CD30+ anaplastic large-cell lymphoma
- Peripheral aborising and polymorphous vessels
- Pink-yellow structureless background
What are the complications of primary cutaneous anaplastic large-cell lymphoma?
- Extracutaneous involvement — 10% involve lymph nodes; visceral involvement is rare occurring 2 months to 10 years after initial diagnosis
- Association with lymphomatoid papulosis
- Impact on quality of life
How is primary cutaneous anaplastic large-cell lymphoma diagnosed?
The diagnosis of primary cutaneous anaplastic large-cell lymphoma requires careful correlation of history, examination, and histopathology. Staging of pcALCL uses the TNM (Tumour, Nodes, Metastases) system.
Recommended investigations include:
-
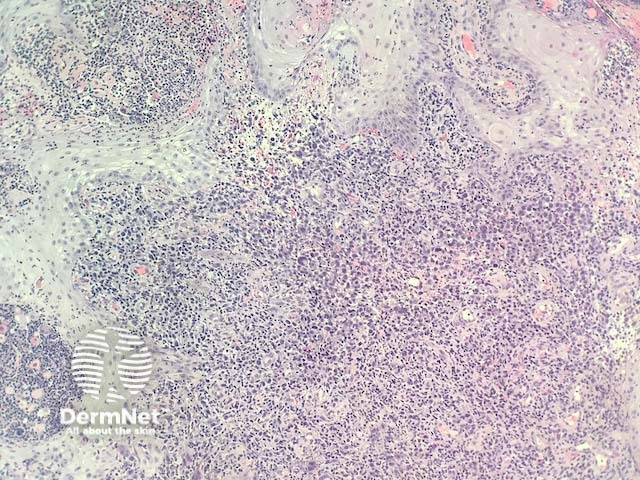
Skin biopsy for histopathology and immunohistochemistry
- Sheets of large irregular polygonal CD30+ cells throughout the dermis and sometimes extending into the subcutis
- Dermal lymphatic involvement is frequent
- ‘Hallmark’ cells are sometimes seen
- Pseudocarcinomatous epidermal hyperplasia [see Pseudocarcinomatous hyperplasia in anaplastic large cell lymphoma pathology]
- At least 75% of tumour cells are CD30 positive
- T-cell receptor (TCR) gene rearrangement to assess clonality; a clonal TCR gene rearrangement is found in 60–100% of cases
- Complete blood count and differential
- Comprehensive metabolic panel
- Lactate dehydrogenase
- Contrast enhanced CT scan and/or PET/CT for disease staging
- Excisional biopsy of any avid or clinically suspicious lymph node >1.5cm
- Bone marrow biopsy should be considered in the setting of multifocal generalised skin lesions, haematological abnormalities on blood test, or evidence of extracutaneous disease.
What is the differential diagnosis for primary cutaneous anaplastic large-cell lymphoma?
- Systemic anaplastic large-cell lymphoma
- Transformed mycosis fungoides
- Other systemic T-cell lymphomas with secondary cutaneous involvement including Hodgkin lymphoma and adult T-cell leukaemia-lymphoma
- Lymphomatoid papulosis can be indistinguishable on histology alone
- Nodular reactive lymphoid hyperplasia secondary to insect bites, scabies, medications, and infections [see Cutaneous pseudolymphoma]
What is the treatment for primary cutaneous anaplastic large-cell lymphoma?
Primary cutaneous anaplastic large-cell lymphoma is usually treated by surgical excision or radiotherapy of solitary or few nodules.
Treatment options for extensive cutaneous disease or regional lymph node involvement include:
- Brentuximab vedotin — an anti-CD30 monoclonal antibody linked to cytotoxic monomethyl auristatin E is the preferred option but up to 65% of patients develop a peripheral neuropathy
- Others — methotrexate, bexarotene, pralatrexate (analogue of methotrexate).
Multi-agent chemotherapy, such as CHOP, is not considered first-line therapy due to high rates of rapid relapse and significant toxicity compared to other systemic options.
What is the outcome for primary cutaneous anaplastic large-cell lymphoma?
Primary cutaneous anaplastic large-cell lymphoma typically has an indolent course despite the malignant appearance on histology. The five-year survival has been estimated to be 95%, but this may be as low as 50% for generalised cutaneous or extracutaneous disease.
Partial or total regression of pcALCL occurs in 20–40% after a median period of 2 months (range 1–6 months).
Good prognostic indicators include:
- Age under 60 years
- Spontaneous regression.
Poor prognostic indicators:
- Age over 60 years
- Extensive involvement of limbs, particularly the legs
- Extracutaneous disease.
Ongoing clinical surveillance is recommended to monitor for recurrence or extracutaneous spread. Up to 50% of cases recur. Extracutaneous spread has been reported in 25% of recurrences, with half of those involving only local lymph nodes.
Bibliography
- Brown RA, Fernandez-Pol S, Kim J. Primary cutaneous anaplastic large cell lymphoma. J Cutan Pathol. 2017;44(6):570–7. doi:10.1111/cup.12937. Journal
- Kartan S, Johnson WT, Sokol K, et al. The spectrum of CD30+ T cell lymphoproliferative disorders in the skin. Chin Clin Oncol. 2019;8(1):3. doi:10.21037/cco.2018.12.03 Journal
- Milan E, Miceli P, Sernicola A, Finotto S, Marino D, Alaibac M. Complete remission of primary cutaneous anaplastic large cell lymphoma after a short course of brentuximab vedotin. Mol Clin Oncol. 2021;14(6):121. doi:10.3892/mco.2021.2283. PubMed Central
- Moodley N, Nombona P, Mosam A. Primary cutaneous anaplastic large-cell lymphoma. Dermatopathology (Basel). 2019;6(2):163–9. doi:10.1159/000500259. PubMed Central
- Uzuncakmak TK, Akdeniz N, Karadag AS, Taskin S, Zemheri EI, Argenziano G. Primary cutaneous CD 30 (+) ALK (-) anaplastic large cell lymphoma with dermoscopic findings: a case report. Dermatol Pract Concept. 2017;7(1):59–61. doi:10.5826/dpc.0701a12. PubMed Central
- Willemze R, Cerroni L, Kempf W, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas [published correction appears in Blood. 2019 Sep 26;134(13):1112]. Blood. 2019;133(16):1703–14. doi:10.1182/blood-2018-11-881268. Journal
- Xavier Júnior JCC, Ocanha-Xavier JP. Cutaneous T-cell lymphomas in the revised 4th edition of World Health Organization classification of tumors of hematopoietic and lymphoid tissues (2017). An Bras Dermatol. 2018;93(6):871–3. doi:10.1590/abd1806-4841.20188057. Journal
On DermNet
- Cutaneous pseudolymphoma
- Cutaneous T-cell lymphoma
- Lymphomatoid papulosis
- Primary cutaneous CD30+ lymphoproliferative disorders
- Pseudocarcinomatous hyperplasia in anaplastic large cell lymphoma pathology
- Skin manifestations of haematological diseases
Other websites
- Primary cutaneous anaplastic large-cell lymphoma — Cutaneous Lymphoma Foundation
