Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Diagnosis and testing Terminology
Author: Brian Wu PhD. MD Candidate, Keck School of Medicine; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, July 2015.
Immunohistochemistry (IHC) is considered to be an advanced form of histopathology. Immunohistochemistry is not usually used initially but is added when routine/regular histological testing is insufficient to form a diagnosis.
IHC uses primary antibodies to label a protein, then uses a secondary antibody which is bound to the primary one. In immunoperoxidase staining, an antibody is joined to an enzyme, peroxidase, that catalyses a reaction in which the protein is specifically stained brown. IHC can also involve fluorescently labelled antibody so that when viewed under a light microscope a certain pattern will be observed from the emitted fluorescence.
The IHC pattern is considered diagnostic, demonstrating nuclear, membranous or cytoplasmic patterns. IHC is often used in situations where a presence or absence of certain proteins can form a basis for a diagnosis. It can also be used to distinguish between two different disease processes that may otherwise appear similar to the pathologist.
The most common process of preparing immunohistochemical slides is as follows:
The advantages of IHC include:
The disadvantages of IHC are as follows:
Hundreds of immunohistochemical stains are used to identify different tumours and other neoplasms. Just a few of the IHC stains used in dermatology are listed below.
IHC Stain |
Uses/Image caption |
|
|---|---|---|
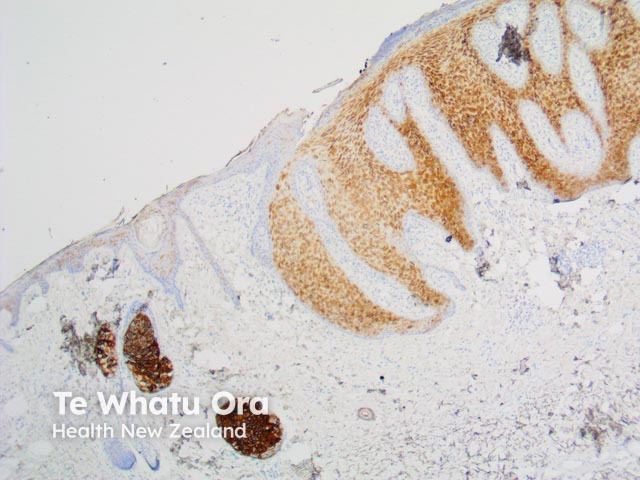
BCL2 |
Used to distinguish between basal cell carcinomas and trichoepitheliomas |
|
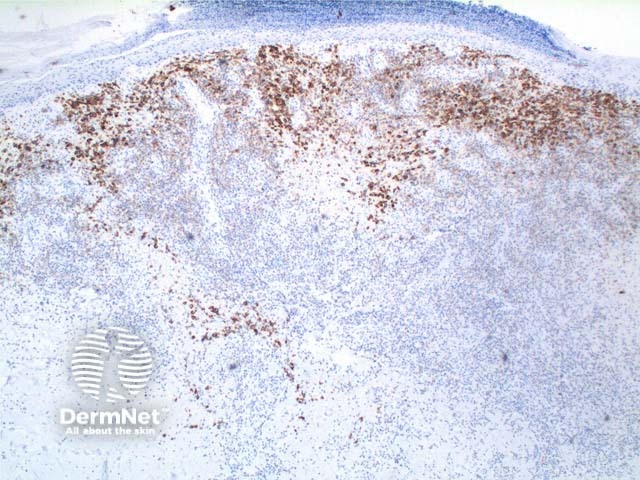
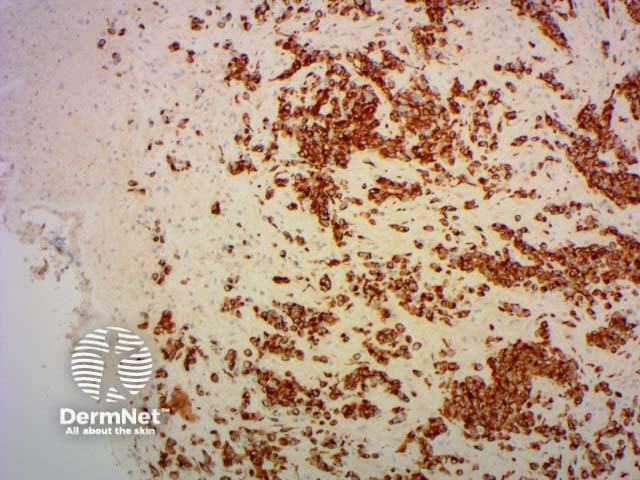
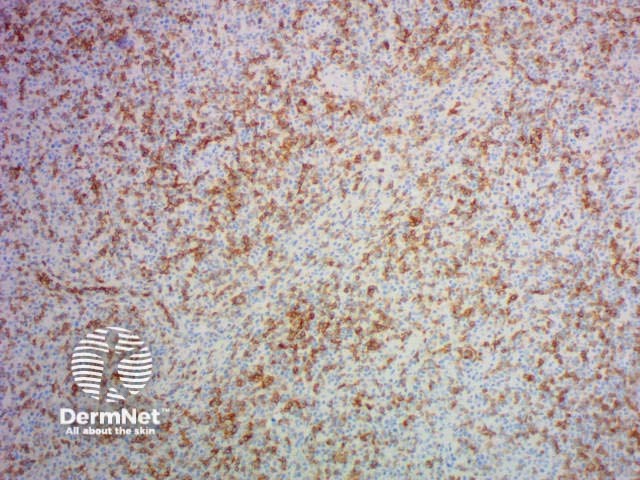
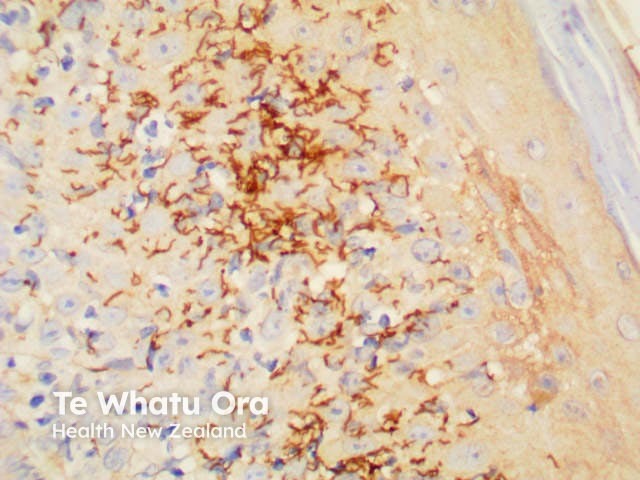
CD3 |
T-cell marker; strongly positive in mycosis fungoides |
|
CD4 |
Helper T-cell marker |
|
CD8 |
Suppressor T-cell marker |
|
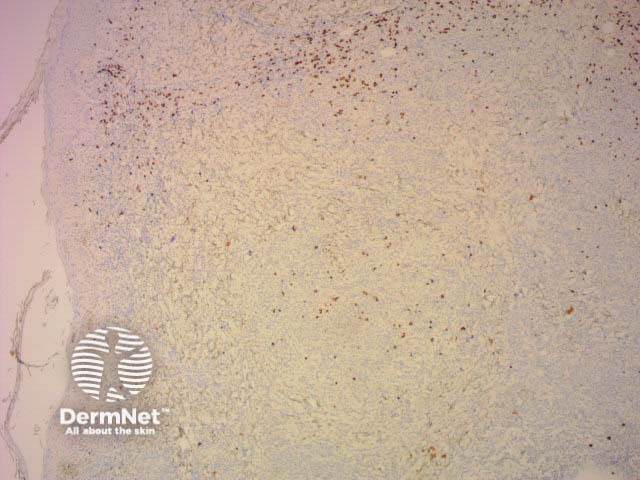
CD20 |
B-cell marker |
|
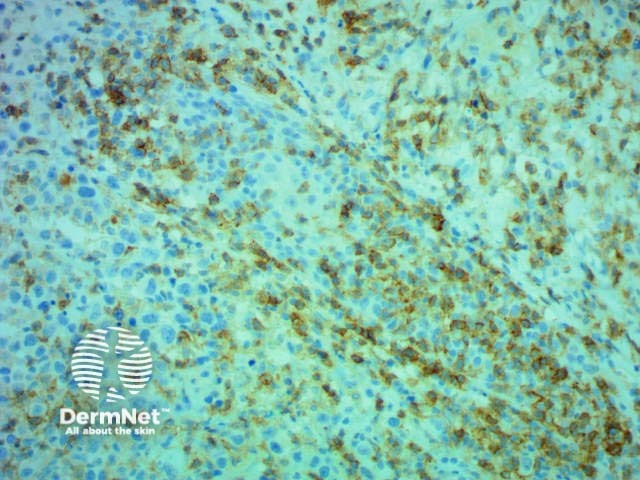
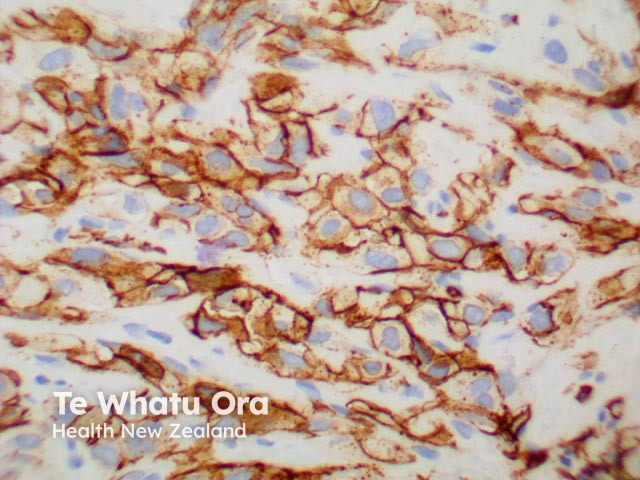
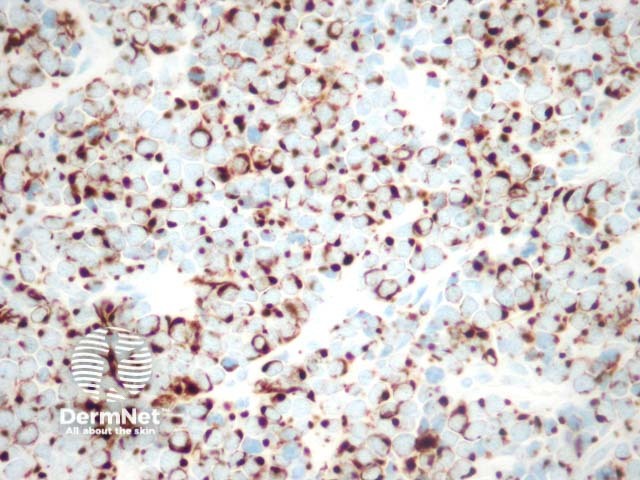
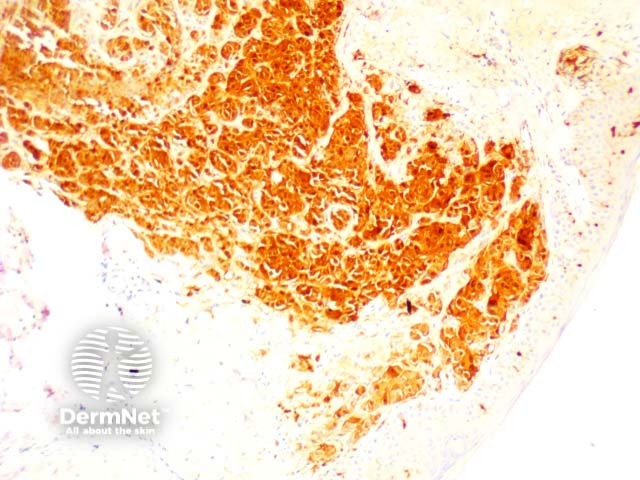
CD30 |
Can be used in the diagnosis of Hodgkin lymphoma and anaplastic lymphomas. Large cells: Golgi apparatus and membranous staining |
|
CD31 |
Helps to identify endothelial tumour |
|
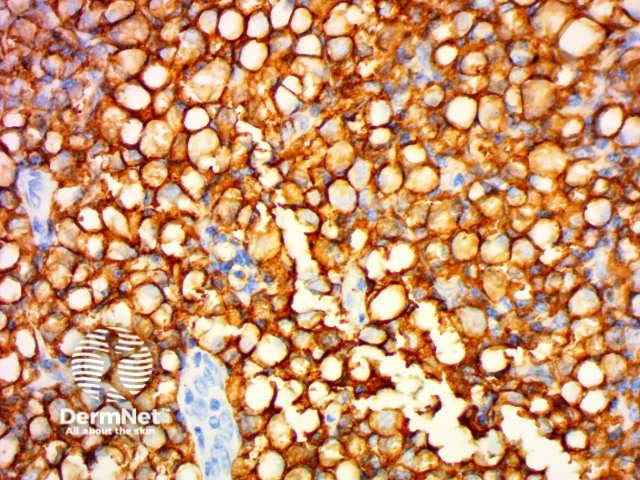
CD34 |
Distinguishes different endothelial tumours and is positive in dermatofibrosarcoma |
|
CD56 |
Used in the diagnosis of non-Hodgkin lymphomas, leukaemias and small cell carcinomas |
|
CD117 |
Marker for KIT receptor and positive in various tumours including mastocytosis |
|
CDKN2A (p16) |
Tumour suppressor marker positive in HPV-associated tumours, actinic keratoses and squamous cell carcinoma |
|
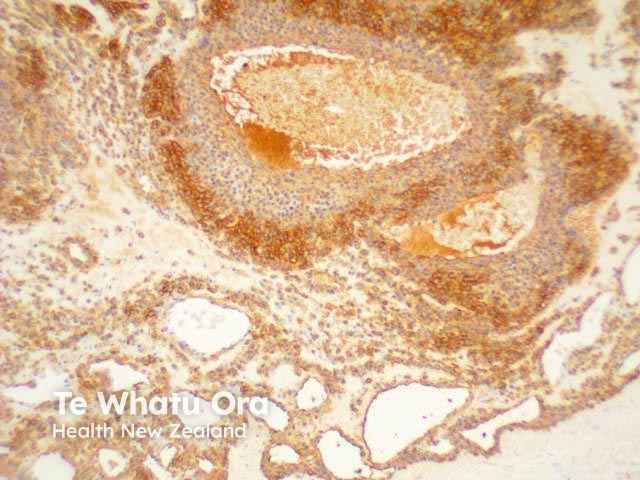
CK (various) |
Cytokeratins can be used to help distinguish benign from malignant adnexal tumours |
|
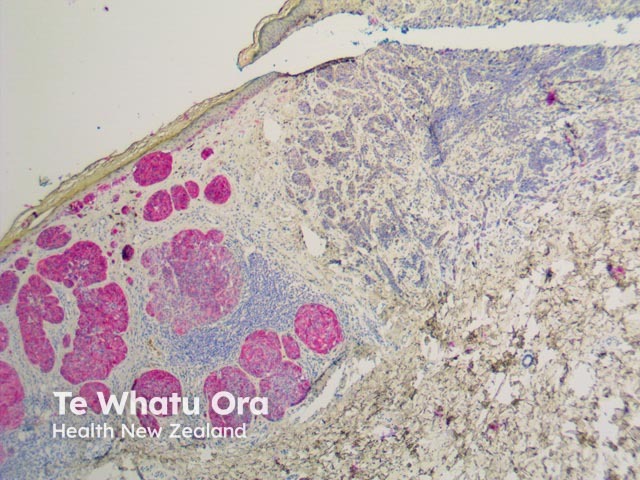
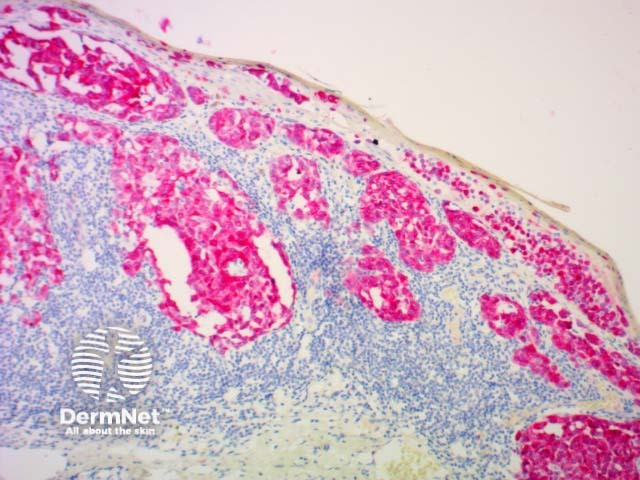
CK 20 |
Specific for Merkel cell carcinoma. Can help identify adenocarcinomas of the gastrointestinal and reproductive system as well as gastrointestinal epithelial tumours |
|
Cytokeratin High Molecular Weight |
Used to detect ductal carcinomas, squamous cell carcinomas and other epithelial neoplasms |
|
Desmin |
Muscle marker |
|
EMA |
Used to identify eccrine neoplasms, Paget disease and sebaceous carcinomas |
|
Factor 13 |
Can help clinicians distinguish between dermatofibrosarcoma and dermatofibroma |
|
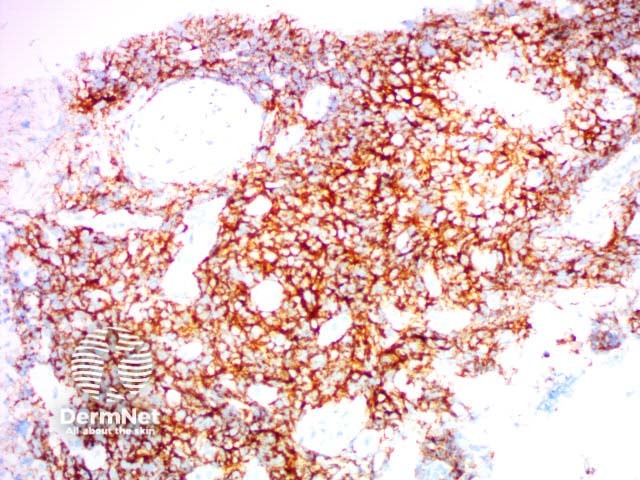
HHV8 |
Human herpesvirus 8 |
|
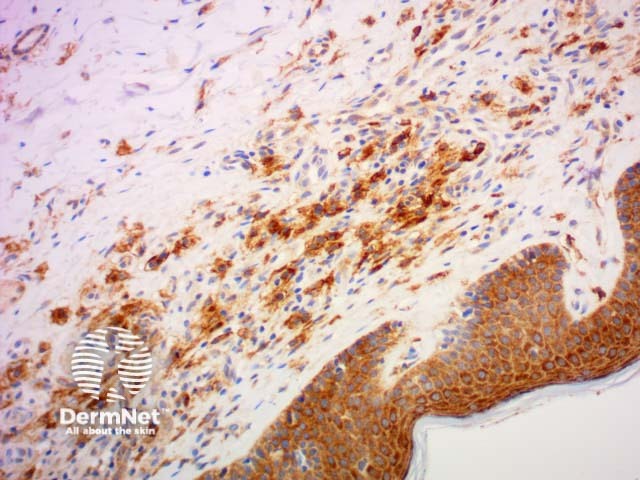
HMB 45 |
Used to detect melanocytes, especially in melanoma but negative in desmoplastic melanoma |
|
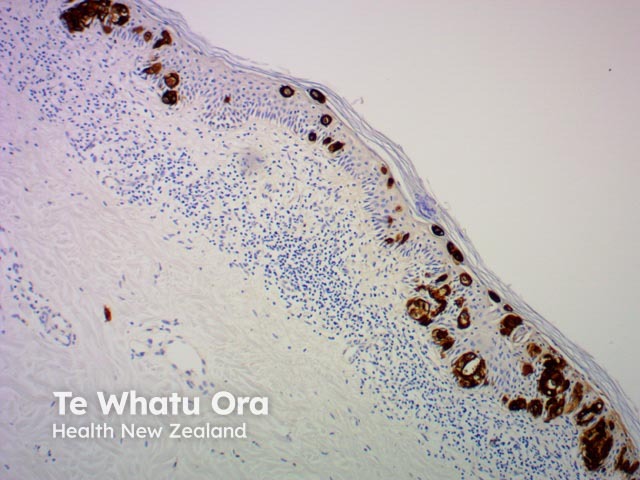
Melan-a |
Can help identify melanocytic naevus cells and melanomas |
|
PDL1 |
Programmed death-ligand 1 |
|
S-100 |
Used to mark tumours of the melanocytes, both naevi and melanoma |
|
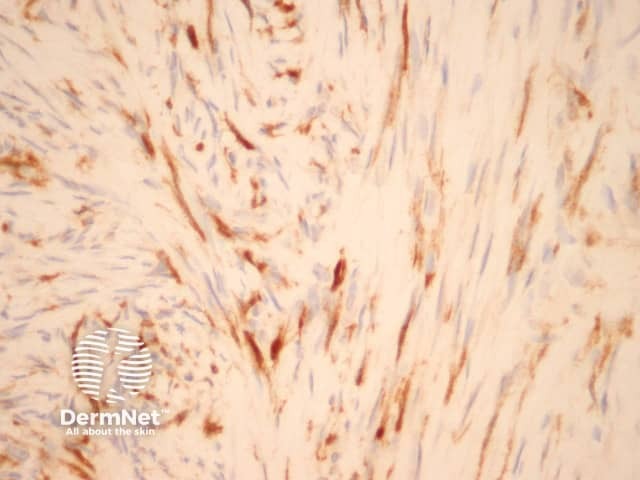
SMA |
Smooth muscle antigen |
|
SOX-10 |
Nuclear marker for melanocytic tumours |
|
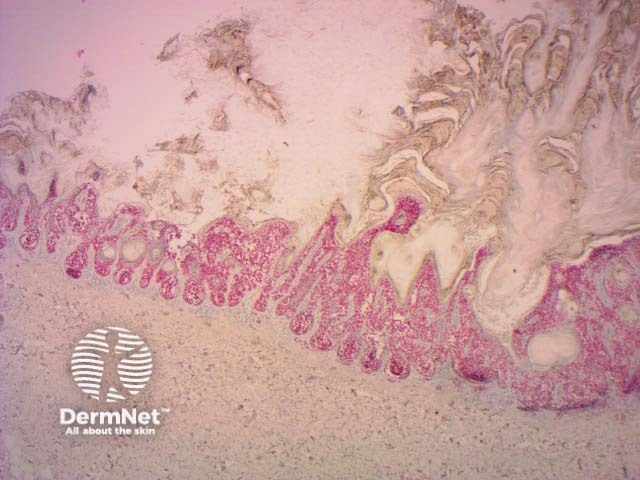
Treponema pallidum |
Demonstrates organisms in secondary syphilis |
|

BCL2
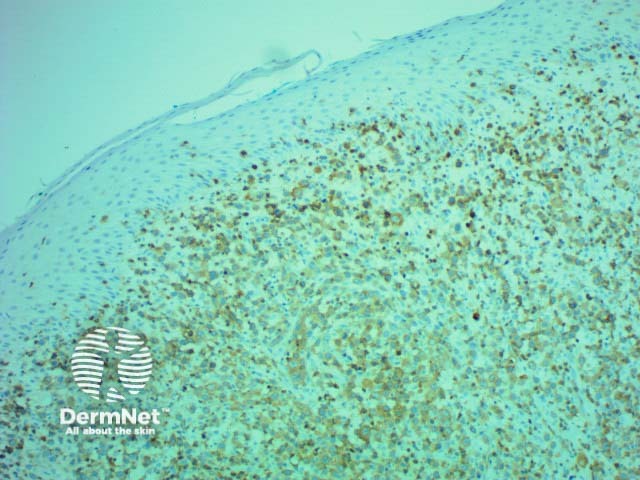
CD3
CD4
CD8
CD20
CD30
CD31
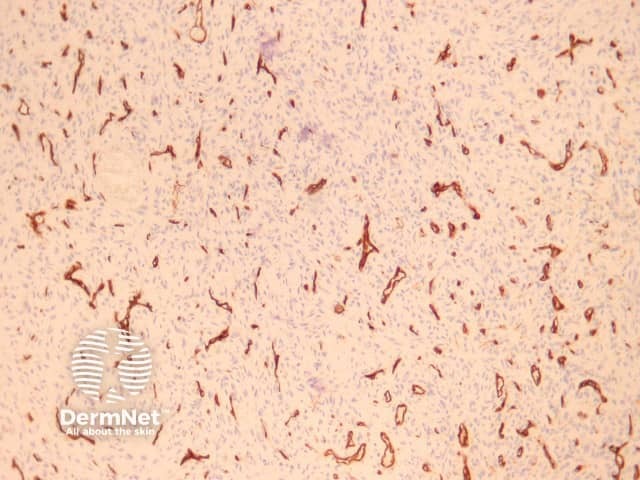
CD34
CD56
CD117

CDKN2A-P16

CK
CK20
CK7
Desmin
EMA
Factor 13a

HHV8
HMB45
Melan A
PDL1
S100
SMA
SOX10
Treponema pallidum