Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Jennifer H Taylor, Dermatology Registrar, University Health Network, Toronto, Canada. DermNet Editor-in-Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, New Zealand, July 2020. Minor update September 2023.
Introduction - human microbiome
Introduction - gut microbiome
Factors affecting gut microbiome
Lifestyle factors affecting the microbiome
Function
Short-chain fatty acids
Connection between gut microbiome and immune system
Probiotics, prebiotics, and synbiotics
Role in skin disease
Our bodies share a symbiotic relationship with trillions of microbes including bacteria, fungi, mites, and viruses. Together, they make up the microbiome, which resides in particular areas of the body such as the skin and gut.
These microbes do not cause harm under normal conditions but directly influence the body’s normal function and disease processes.
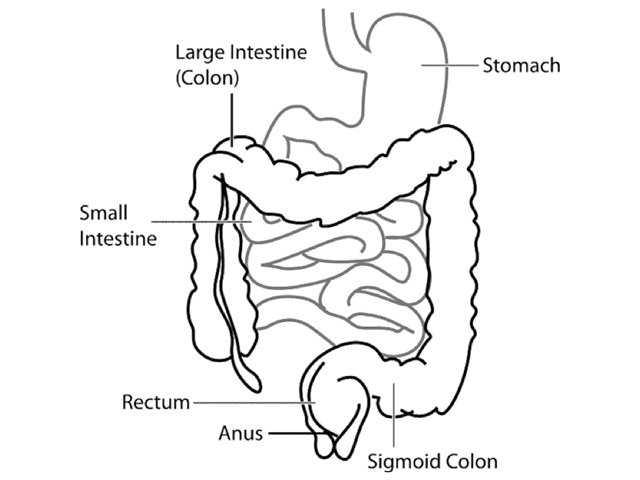
Human gastrointestinal tract
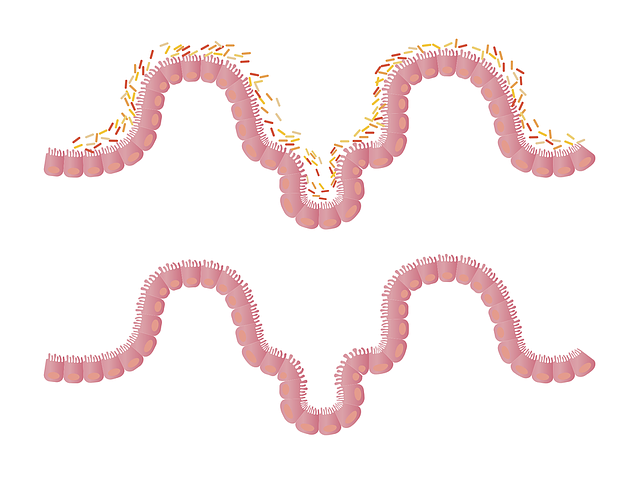
Representation of the intestinal lining with and without microbiota
The mucosal lining of the gastrointestinal tract is home to millions of organisms. Its composition varies with Bacteroidetes, Firmicutes, Actinobacteria, and Proteobacteria dominating the gut microbiome of adults.
The relationship between the gut microbiome and immunity is currently a major topic of research.
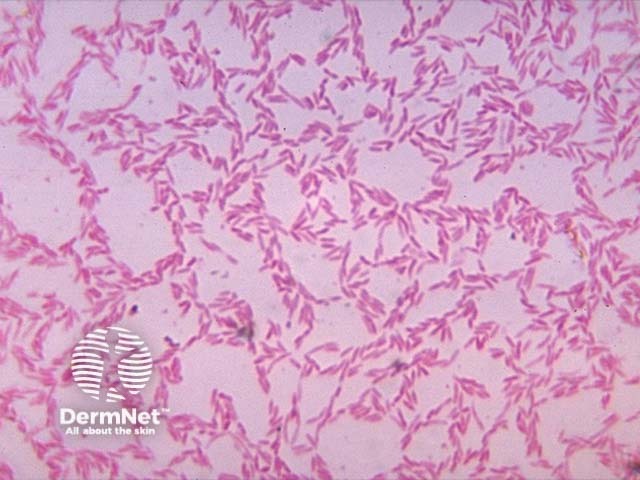
Bacteriodes
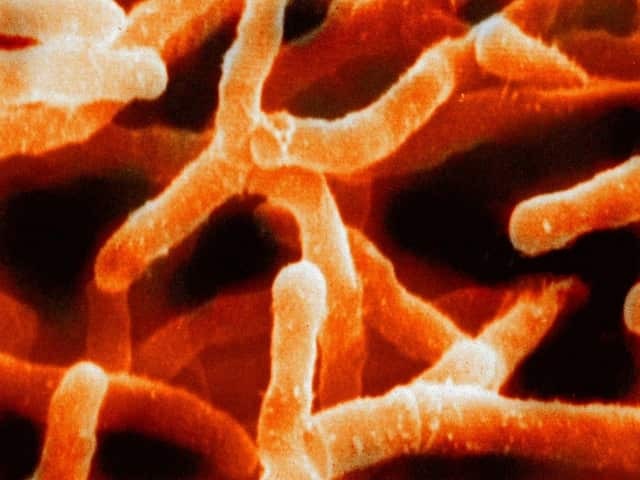
Actinomyces israelii
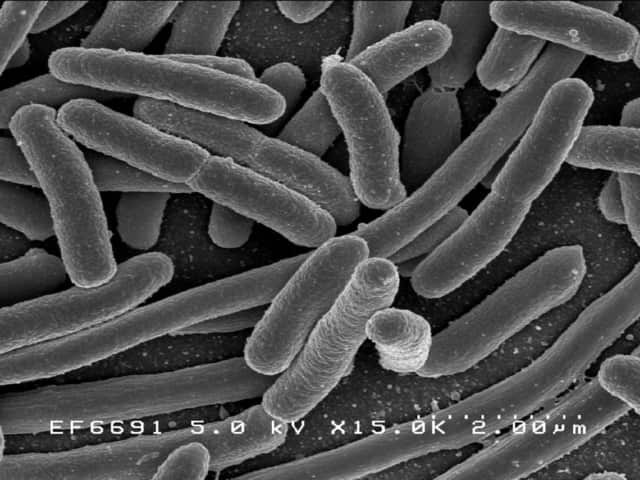
Escherichia coli
The gut microbiome changes over the first three years of life before forming a relatively stable composition. It also varies greatly from person to person and is dynamic within an individual over time. Factors that influence the gut microbiome include:
A widely diverse gastrointestinal and skin microbiome enhances resilience against infection, allergies, autoimmune disease, cancer, ageing, and degenerative diseases. The following lifestyle measures can help achieve this:
Alongside fruit and vegetables, the Mediterranean diet suggests whole grains; lentils/legumes; healthy fats, such as nuts, seeds, and extra virgin olive oil; moderate amounts of fish; some white meat, dairy, few eggs and up to once weekly red meat; red wine in moderation eg, one unit 2-3 times weekly. The green Mediterranean diet is even more rich in plant-based foods and may be more impactful.
The gut microbiome has several important roles in health, particularly in metabolism and the immune system. These include roles in:
One important function of microbes in the gut flora is the production of short-chain fatty acids via the break-down of complex carbohydrates in food. Examples of short-chain fatty acids are propionate, acetate, and butyrate.
Short-chain fatty acids are thought to:
Alterations in the gut composition, the diversity of the microbiome, and abnormal immune reactions to the microbes may result in changes to the immune and regulatory functions of the gut. These changes may ultimately lead to local or systemic immune dysfunction affecting the skin.
Disruption in the gut microbiome has been associated with allergic, inflammatory, autoimmune, metabolic, neuropsychiatric, and neoplastic diseases.
The gut and the skin are suspected to have a bidirectional relationship involving a combination of neurological and immunological responses to changes in the microbiot. Mechanisms by which the gut flora is thought to influence the skin include:
Some studies have observed that gut dysbiosis (microbial imbalance) precedes the onset of atopic dermatitis. Although the relationship is not clear, there are distinct differences in the gut microbiome between people with and without atopic dermatitis.
Infants who go on to develop atopic dermatitis have been reported to have:
Observed changes in microbial composition between individuals with and without acne may be due to:
Small studies have reported possible associations of alterations in the gut microbiome with rosacea, psoriasis, and wound healing.
Probiotics are defined by the World Health Organisation (WHO) as “live microorganisms which when administered in adequate amounts, confer a health benefit on the host”. The most commonly used bacteria in probiotics are Lactobacilli and Bifidobacteria.
Prebiotics are non-digestible fibres that stimulate certain beneficial bacteria in the gut. The most common of these are non-digestible oligosaccharides.
Synbiotics are a combination of probiotics and prebiotics.
The main role of probiotics and prebiotics is to restore and encourage the production of beneficial microorganisms in the gut. Research is focusing on their therapeutic potential and results to date have been conflicting.
The role of probiotic supplements in the prevention of atopic dermatitis is being investigated in pregnancy and infancy to determine if they can improve or help prevent skin disease. Probiotics have not been shown to treat established dermatitis.
It has been reported that probiotics may lead to an improvement in acne by reducing inflammation and decreasing ceramide production.