Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
Describe:
Many general practitioners perform minor surgery for benign and small malignant skin lesions. We strongly recommend that you attend regular hands-on workshops in skin surgery to develop and maintain surgical skills. This course does not replace the need for practical training and experience.
To ensure safe practice, aim to comply with published office surgery standards, especially those of Standards New Zealand – ‘The Essential Standards for Health and Disability Services’, include:
Skin surgery is indicated for the removal of skin lesions that are, or may be, malignant, or if benign, are causing concern because of symptoms or cosmetic appearance.
Patients with large lesions or lesions on the face may be referred to a dermatologist or plastic surgeon for management.
The surgical management of benign and malignant skin lesions may include:
Combinations of these techniques are often used.
The choice of procedure depends on:
The aim is for minimal scarring after any surgical procedure. To achieve this, the excision should occur at right angles to the direction of the resultant pull of the muscles or parallel to natural skin creases and wrinkles – the more creases and wrinkles the less obvious the scar.
Scars are initially red and firm. In time (usually 3 to 12 months), the induration and erythema lessen leaving a soft scar, paler than surrounding skin. Scars tend to stretch, especially when there is loss of skin and obvious wound tension. More conspicuous scarring arises in the following circumstances:
Coronary artery bypass After wound infection Gravel abrasions 


Suture marks are more prominent in coarse oily skin, for example on the nose, and less obvious in hairless skin such as the margin of the lips, and are less likely with early removal of sutures.
Topical anaesthesia may be useful for:
This may be delivered as freezing spray at the time of the procedure (ethyl chloride, nitrous oxide or very light liquid nitrogen), or as a cream applied an hour or two earlier – such as eutectic mixture of prilocaine and lidocaine (EMLA 5% Cream or patch) or amethocaine hydrochloride (Ametop™ Gel).
Most skin procedures require intradermal anaesthetic. Lignocaine (Xylocaine™), an amide, is most commonly used. The onset of action is rapid (one to two minutes) and it lasts one to three hours. The addition of adrenaline 1:100,000 prolongs its duration, reduces toxicity and controls bleeding. The adrenaline should not be used for circumferential block of a digit or penis, or in those with impaired peripheral circulation or serious heart disease.
The maximum safe volume of 1% plain lignocaine in an adult on a single occasion is about 20ml; detailed safety information can be found on manufacturers' data sheets on the Medsafe website. It may be injected using 1 to 5 ml syringe and 23 to 30 gauge needle, or using dental syringe, 30 gauge disposable dental needle and 2.2 ml cartridge.

EMLA cream

Vasoconstriction from EMLA

Infiltrating local anaesthetic

Dental syringe
Methods of haemostasis include:

Haemostatic solution
Electrosurgery is used for haemostasis and desiccation of tissue using high frequency (0.1-1 MHz), high voltage, and low-amperage currents in a modulated manner. It should in general be avoided in those with pacemakers although modern units are probably quite safe in stable patients providing the path of the electric current does not pass through the heart.
For sterility, disposable tips or needles are used with the hand piece inserted in a sterile glove or specific polythene casing. Reusable tips should be sterilised in an autoclave.
Methods include:

Electrosurgery trolley

Hyfrecator®
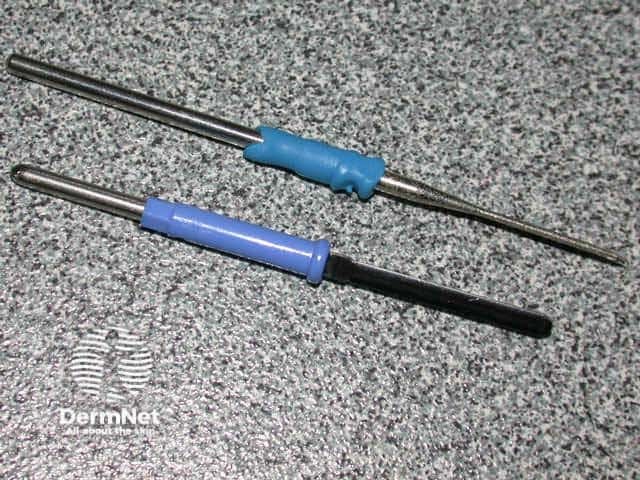
Sharp and blunt disposable tips
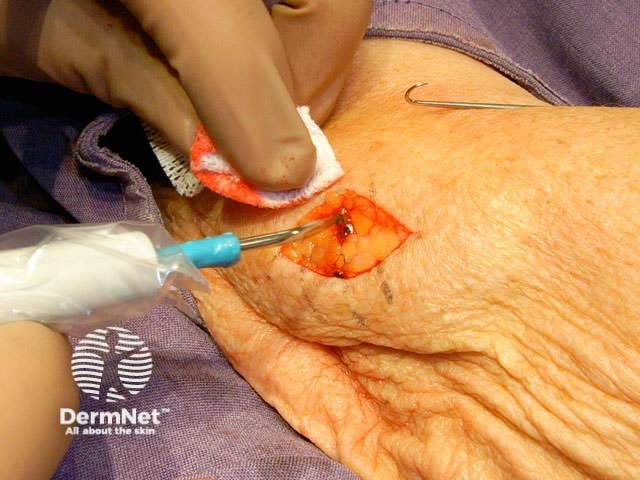
Haemostasis
Electrocautery uses red-hot wire to burn the tissue. Hand-held disposable and mains-powered heavy duty units are available.
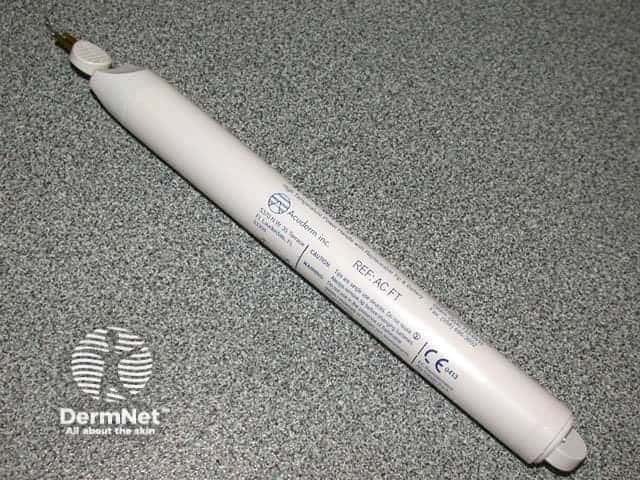
Hand-held cautery

Geiger® cautery set

Cautery tips
| Skin lesion | Electrosurgical method |
|---|---|
| Skin tags, warts, syringomas | Gentle electrodessication prior to curettage |
| Telangiectasia | Fine needle electrode and very low power electrodesiccation |
| Small non-melanoma skin cancers (dermatologists) | Shave, curette the lesion prior to electrofulguration / desiccation or cautery (always send specimen for histology) |
Information for patients
See the DermNet bookstore