Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Dr Jamie Banks, Department of Plastic and Reconstructive Surgery, St George’s University Hospitals, U.K. (2023)
Previous contributors: Dr Sonya Havill, Dermatologist, New Zealand (2002)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction Purpose Types of skin grafts How it works Complications Graft failure Scarring
A skin graft consists of skin taken from one part of the body to cover an area where skin is missing or damaged. This may follow surgical removal of skin cancer or an injury such as a burn or other trauma.
Unlike ‘flap’ reconstruction which has its own intrinsic blood supply, a skin graft is a free piece of tissue which receives blood supply from the bed onto which it is grafted and therefore its survival relies on the integrity of the underlying wound bed.

Excised wound immediately prior to the procedure (SG-patient9)
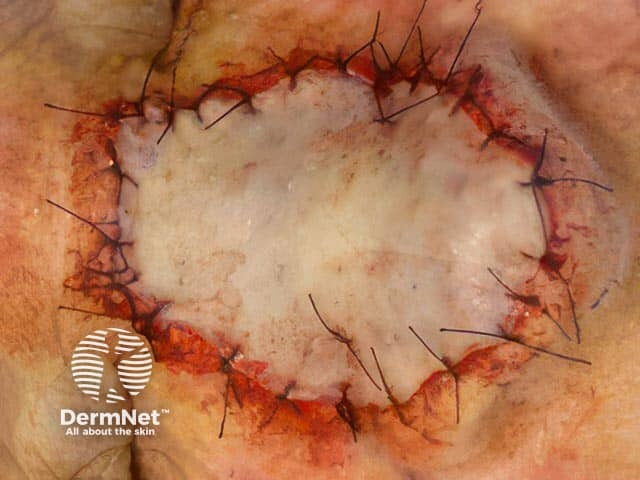
Grafted wound immediately after the procedure (SG-patient9)

The established full thickness skin graft after skin cancer removal on the nose (SG-patient9)
A skin graft is required when the area of skin loss is too big to be closed using local skin and stitches alone. While with very superficial wounds, the cells that create the new top layer of skin remain intact, in deeper wounds (such as full-thickness excisions of skin cancers), this layer is lost and the surgeon may need to kickstart the healing process with a graft of healthy skin cells from elsewhere.
The skin graft covers the wound, attaching itself to the cells beneath, and begins to grow in its new location. Similarly, a skin graft may be used after removal of a skin cancer if the dermatologist or surgeon is worried that they may need to return to take a further margin of tissue to ensure clearance. If a skin graft wasn’t performed, the area would be an open wound and take much longer to heal.
Split-thickness skin grafts (STSG) are also known as split skin grafts (SSG) or partial-thickness skin grafts.
This type of graft is taken by shaving a very thin surface layer (epidermis and a variable thickness of dermis) of the skin with a special machine called a dermatome, or manually with a large knife. The machine is powered by air and quite noisy. The shaved piece of skin is then applied to the wound.
STSGs may then be meshed to increase the area they can cover and their ability to contour to the defect. The donor site heals on its own with dressings over a few weeks.
A full-thickness skin graft (FTSG) is taken by removing all the layers of the skin down to the fat with a scalpel. It is done in a similar way to skin excision. The piece of skin is cut into the correct shape, then applied to the wound.
Since it includes the full layer of dermis, it has a better cosmetic outcome than a split-thickness graft, less contraction (shrinkage) over time, and more resistance to subsequent trauma. However, due to the increased thickness, FTSGs initially have a lower chance of graft survival. They are also limited by the size of the donor site, as harvesting leaves a full-thickness defect that must itself be managed and stitched closed.
Composite grafts are a specialist type of graft used in some unique situations. They include all the skin layers, as well as some of the underlying fat, and can include underlying cartilage from the donor site. They can be used to reconstruct fingertips following traumatic amputation (using the amputated part to provide the graft) or to reconstruct special areas like the nasal tip after removal of skin cancers. Broadly speaking, their post-operative management is similar to full-thickness skin grafts.
The above examples describe autografts, where the graft is taken from the person who will receive it. Cadaveric grafts are an allograft, where the graft is taken from an organ donor. These, along with xenografts (taken from a different species such as porcine/pig grafts), can trigger the recipient’s immune system to reject the tissue over time. As such, they are preserved for use in acute trauma, typically following massive burns, as a temporising measure until sufficient autograft can be sourced.
Taking this a step further, cadaveric grafts can also be used as a dressing on top of an autograft to improve the chance of the underlying autograft succeeding in very unwell patients, in a novel process known as sandwich grafting.
A range of skin substitutes are also available for reconstruction instead of, or in combination with, skin grafts:
CEA (cultured epidermal autograft):
A sample of skin tissue is taken and grown in the lab over a three-week period into a new epidermis, before being applied in a manner similar to a thin split-thickness graft. Unsurprisingly, these very thin grafts are very susceptible to damage and often require longer immobilisation to prevent shear forces and graft loss. They are expensive and require a growth phase before use.
ASCS (autologous skin cell suspension):
This uses a similar technique to CEA, but applies the newly grown cells as a spray rather than as a preformed graft.
Dermal substitutes:
This is used to reconstruct the dermis, serving as temporary or permanent scaffolds that promote wound healing and facilitate the regeneration of new tissue. They can be synthetic or biological, with the latter’s collagen derived from human or animal sources. This is gradually replaced by the recipient’s own collagen to support a subsequent skin graft.
These substitutes can be applied over areas that would not usually form an adequate wound bed to receive a graft, such as exposed bone or tendon. This allows for a subsequent split-thickness graft to be applied as a second stage. As with CEA and ASCS, the cost of dermal substitutes limits their use.
Your doctor will explain to you why a skin graft is required, and the process involved. You may have to sign a consent form to indicate that you understand and agree to the surgical procedure.
Tell your doctor:
If the graft is used to cover an area resected due to skin cancer, your surgeon will measure the area of the wound to know what size to make the skin graft. A piece of skin will be shaved or cut from another part of your body (donor site) that is large enough to cover the wound. When possible, skin of similar thickness and colour will be selected. Occasionally, your surgeon may conduct the operation in stages using a tissue expander. This is a device that works like a balloon under the skin to stretch the area and increase the amount of skin that can be subsequently harvested in a graft.
Once harvested, a split-thickness skin graft may be meshed, where the graft is turned from a continuous sheet into a mesh that looks like a fishing net. This allows a smaller donor site to cover a larger area, improves the contouring to underlying graft bed (which increases the chance of the graft succeeding), and prevents build-up of fluid under the graft. When the dressing is first removed, the graft will look like a criss-cross pattern, but the holes will fill in with time to appear similar to the surrounding skin. Grafts may also be ‘fenestrated’ where small holes are cut to reduce the risk of blood building up underneath the graft, but traditionally fenestration does not increase the area that a graft can cover.
The piece of skin (the graft) will be applied to the wound and is usually secured in place with stitches or surgical staples. A special spongy dressing will be applied directly over the skin graft and often sutured in place. An outer pressure dressing will then be applied to protect the wound. Sometimes a vacuum dressing (known as topical negative pressure therapy) is used for large grafts.
You will have two wounds, the site of the original lesion and the donor site. They may become tender after an hour or two when the effect of the local anaesthetic wears off.
Skin grafts are very fragile and great care must be taken when looking after them.
Split-thickness graft donor sites take about two weeks to heal, whereas full-thickness graft donor sites typically heal a little faster, between 5–7 days. The graft itself ought to develop its new blood supply in 5–7 days; it can take as long as 1–2 years until the area fully settles.
Sometimes the skin graft does not survive the transfer to the new site. This usually happens within the first two weeks after the procedure. It can happen for a variety of reasons including the accumulation of blood or fluid underneath the graft, and/or wound infection.
If this happens, a repeat skin graft procedure may be suggested, or the wound may be dressed regularly and left to slowly heal on its own. It is quite normal for the graft to appear dark, bruised, and crusted on the surface when the dressings are removed early on. This does not necessarily mean it has failed.
In some instances, your doctor may advise against a skin graft at all and opt for prolonged dressings until the wound heals. These situations can include chronic wounds which would be a poor recipient site for a skin graft, scarred or irradiated areas (after radiotherapy), and joints or areas with high mobility where the graft would almost certainly shear and fail.
It is impossible to cut the skin without scarring to some degree. The final cosmetic result depends on the type of skin graft, the location, the size and depth of the wound, and patient factors. Because skin grafts are effectively a patch without their own blood supply and sometimes of less thickness than the wound they are applied to, the final appearance may not be as close to normal as it would be if the wound was able to be closed in a straight line or with a skin flap. The grafted area may look paler and flatter than the surrounding skin with time.
You will have two scars: the scar where the skin graft has been applied, and the donor site. The donor site for a full-thickness skin graft will usually be closed in a straight line with stitches. The donor site for a split-thickness graft will consist of a superficial graze and will heal itself more slowly (initially under a special dressing).
Some people have an abnormal response to skin healing resulting in larger scars than usual (keloid or hypertrophic scarring).