Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lesions (cancerous) Lesions (benign) Diagnosis and testing
Author: Naomi Ashman, Dermoscopist, Torbay Skin, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. June 2019.
Introduction Clinical features Dermoscopic features Differential diagnoses Histological explanation
Actinic keratosis is a scaly lesion found on sun-damaged skin. It is considered precancerous because a cutaneous squamous cell carcinoma may arise from actinic keratosis. Actinic keratosis is also known as AK and solar keratosis.
Actinic keratosis is an irregular, skin coloured, red or pigmented papule or plaque and is most often found on a bald scalp, ear, face or back of the hand. Multiple lesions are often present. Other features may include:

Actinic keratosis

Actinic keratosis

Actinic keratosis affecting a hand
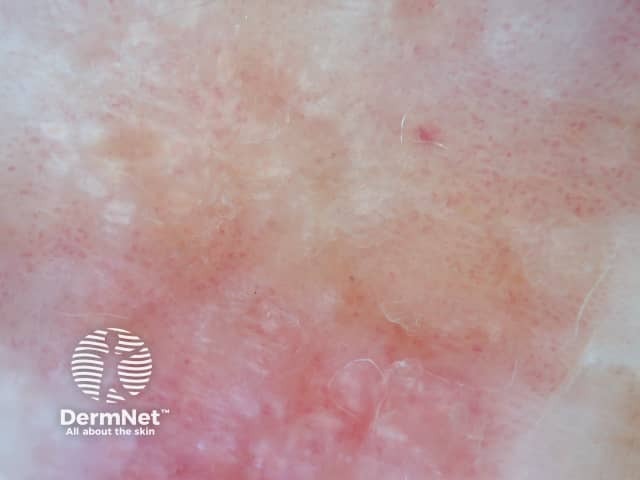
Nonpigmented actinic keratosis on the face is characterised by a 'strawberry pattern' on dermoscopy. The border of the lesion is often well demarcated but may merge into surrounding skin as many patients have extensive sun damage. Other features may include:

Actinic keratosis affecting the face

Strawberry pattern dermoscopy of facial actinic keratosis

Strawberry pattern dermoscopy of facial actinic keratosis
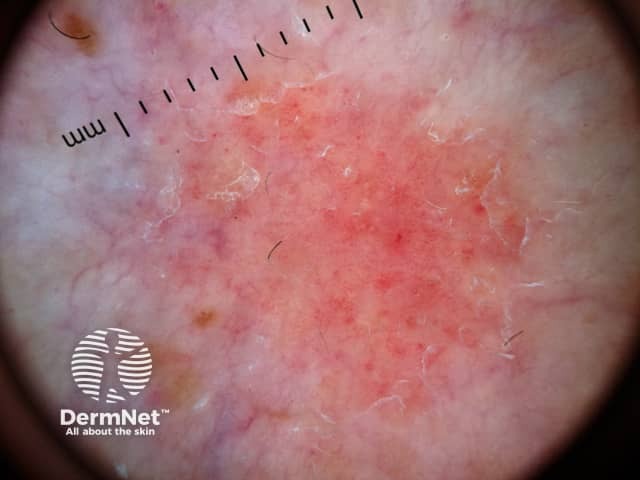
Actinic keratosis on nonfacial skin usually exhibits a nonspecific pattern. Features may include:

Dermoscopy of actinic keratosis on nonfacial skin

Actinic keratosis on nonfacial skin

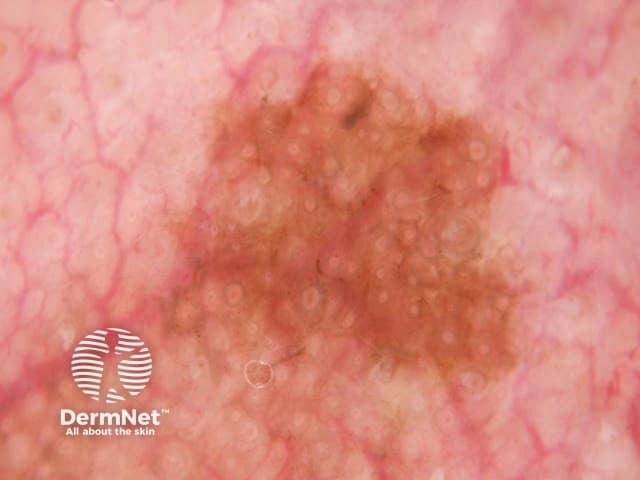
Rosettes in actinic keratosis
Pigmented actinic keratosis has a similar appearance to nonpigmented actinic keratosis with the addition of pigmented structures.
The most common dermoscopic findings are:
Other features include:

Dermoscopy of actinic keratosis
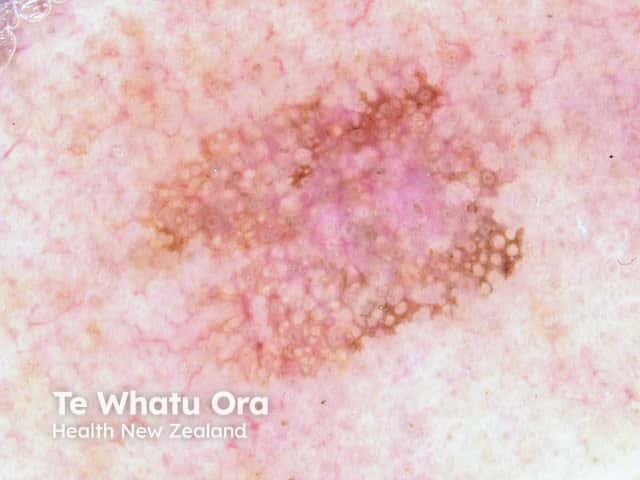
Dermoscopy of pigmented actinic keratosis

Dermoscopy of pigmented actinic keratosis
Actinic keratosis is diagnosed by a combination of clinical and dermoscopic features and sometimes can be difficult to distinguish from other lesions. It may coexist with solar lentigo, cutaneous squamous cell carcinoma, and lentigo maligna.
Cutaneous squamous cell carcinoma can arise from actinic keratosis. Differentiation is determined by dermoscopic findings of peripheral white around a central scaly core (the original actinic keratosis).
Dotted/coiled vessels tend to be scattered more randomly in actinic keratosis than in intraepidermal carcinoma where they are arranged in lines or clusters. Vascular structures in squamous cell carcinoma in situ show greater variation in size and structure.
The following four features are significantly associated with lentigo maligna: hyperpigmented follicular openings, obliterated follicular openings, annular-granular structures, and pigmented rhomboids.
Pigmented rhomboids and obliterated follicular openings are significantly more frequent in lentigo maligna than pigmented actinic keratosis.
Lentigo maligna tends to be smooth to the touch, whilst actinic keratosis tends to be rough in texture. The border of lentigo maligna has variable abruptness (fading in some areas, sharp in others) whereas pigmented actinic keratosis tends to have a defined border. Lentigo maligna may have asymmetrical pigmented follicular openings and a darker dot located within ostial openings (a concentric circle or the isobar sign); a finding rarely seen in pigmented actinic keratosis.
Psoriasis presents with red scaly plaques. Occasionally a solitary plaque of psoriasis may be confused with actinic keratosis. It has a regular structure. The uniform scale tends to be whiter and more silvery in psoriasis compared to the irregular yellowish scale of actinic keratosis. Dotted blood vessels are distributed uniformly throughout the lesion in psoriasis.
Dermoscopic view of squamous cell carcinoma

Dermoscopic view of squamous cell carcinoma in situ
Dermoscopic view of lentigo maligna showing pigmented circles and the isobar sign
Dermoscopic view of psoriasis
The correlation between histological and dermoscopic features of actinic keratosis is poor.
The exact histological explanation of rosettes is unclear but they are thought to be due to an interaction between polarised light and narrowed keratin-filled, or fibrotic adnexal openings. Haspeslagh et al found that small rosettes (0.1–0.2 mm) corresponded to concentric horny material in follicular and eccrine ducts at the infundibular level and larger rosettes (0.3–0.5 mm) to perifollicular concentric fibrosis.
Alternating orthokeratosis and parakeratosis.
Vessels between hair follicles, with white haloed follicular openings.
Circles that appear in pigmented keratosis are due to the involvement of follicular infundibula.