Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Anthrax — extra information
Anthrax
Author: Reviewed and updated by Dr Amanda Oakley Dermatologist, Hamilton, New Zealand; and Vanessa Ngan, Staff Writer; June 2014.
Introduction
Demographics
Clinical features
Complications
Investigations
Differential diagnoses
Treatment
Prevention
What is anthrax?
Anthrax is a serious bacterial infection caused by Bacillus anthracis. Untreated, up to one-fifth of infected individuals die of the disease. Prompt treatment with antibiotics is curative and most recover fully.
Anthrax is also called wool sorter's disease, splenic fever, charbon, and milzbrand.
Cutaneous anthrax treated with doxycycline
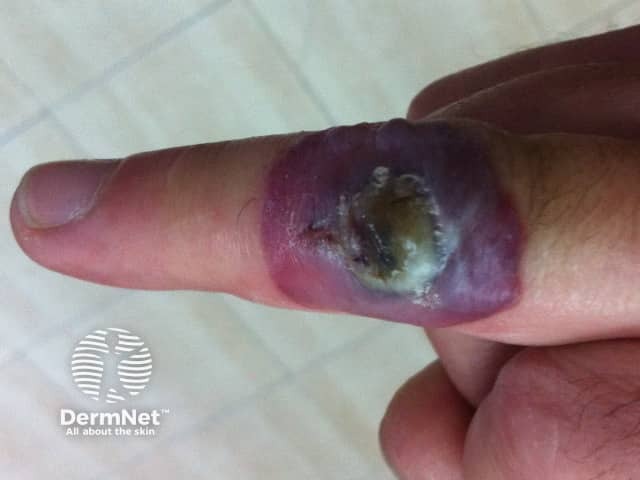
At diagnosis

6 days later

4 weeks after diagnosis
Who gets anthrax and how is it transmitted to humans?
Anthrax is extremely rare in the developed world but sporadically occurs among farmers in Africa, the Middle East and the Caribbean. It can also infect workers in the wool, hair or bristle industries, butchers and gardeners.
Anthrax primarily affects sheep and cattle that ingest spores lying dormant in the pasture. Human infection can arise from spores entering the skin by inoculation through a minor injury, through the lungs by inhalation (wool sorter's disease) or by ingestion. Most anthrax infection (95%) is via the skin (cutaneous anthrax).
What are the clinical features of cutaneous anthrax?
Cutaneous anthrax develops usually between 1-7 days after skin exposure.
- Most often anthrax starts as a localised infection on exposed skin (usually face, hands or arms).
- It looks like an insect bite and is known as a "malignant pustule". Usually painless, an itchy bump appears with surrounding redness. After a day or so, it blisters then ulcerates. At this stage, it is about 1–3 cm in diameter and circular in shape, surrounded by small blisters and marked swelling of the surrounding skin.
- Characteristically, the ulcer develops a black scab, which is called a necrotic eschar. Within a couple of weeks, the infection heals leaving a scar.
The infection occasionally results in a red streak tracking to nearby lymph glands (lymphangitis). These lymph nodes then often swell and become sore.

Lymphangiitis due to anthrax
What are the complications of cutaneous anthrax?
Anthrax becomes dangerous if it spreads widely through the bloodstream. The risk of anthrax spreading through the body is higher if the infection is acquired by inhalation or ingestion.
Symptoms of this include fever, headache and weakness. In mild cases, recovery occurs within three weeks.
In severe infection, prostration, delirium, collapse and death often occur.
What investigations should be done when suspecting anthrax?
- Microscopy – a swab from the infected spot may reveal the characteristic gram-positive B. anthracis under the microscope.
- Serology – Anthrax can also be detected by several types of blood test. However, it often takes several days to get a result.
- Skin biopsy – A pathologist may report markedly swollen skin, haemorrhage, inflammation and abscess formation.
What is the differential diagnosis for anthrax?
The appearance of anthrax can mimic the skin infections due to staphylococci and streptococci, and much less common viral infections due to cowpox, orf and cat scratch disease.
What is the treatment for anthrax?
Cutaneous anthrax is treated with antibiotics. Treatment must be started straight away to reduce the chance of the anthrax spreading from the initial skin lesion.
- Traditionally, treatment has been with intravenous or intramuscular penicillin for 7–10 days. However, for uncomplicated cutaneous anthrax, an oral tetracycline, especially doxycycline, is given in an outpatient setting. It is also suitable for those allergic to penicillin.
- With recent concerns that B. anthracis in the setting of bioterrorism may be resistant to penicillin and tetracycline, a quinolone such as ciprofloxacin is becoming the antibiotic of choice. It is particularly used for inhaled anthrax infection. Initially, it should be given intravenously, and then continued orally for up to 60 days.
In some cases, it is necessary to surgically scrape off the black eschar from the anthrax ulcer. It is essential that this is done with antibiotic cover as interfering with the wound could encourage the spread of the bacteria. If the eventual scar is unsightly, a plastic surgeon may be able to improve its appearance later.
A newer treatment for inhalational anthrax is the monoclonal antibody raxibacumab. It is used as part of combination therapy with appropriate antibiotic agents.
Can anthrax be prevented?
Anthrax spores can survive for over 20 years in dry pasture and soil. Precautionary measures people can take include:
- Wearing long sleeves and protective gloves if handling infected animals.
- Isolating infected cattle and vaccinating herds against anthrax.
- Human vaccination is available for those at significant risk of developing the disease.
For people who have been exposed to anthrax but don’t have symptoms, prophylactic treatment with an antibiotic should be given to reduce the risk of infection. A 60-day oral course of penicillin, tetracycline or quinolone is recommended.
References
- M. K. Karahocagil, N. Akdeniz, H. Akdeniz, Ö. Çalka, H. Karsen, A. Bilici, S. G. Bilgili, Ö. Evirgen (2008). Cutaneous anthrax in Eastern Turkey: a review of 85 cases. Clinical and Experimental Dermatology 2008; 33: (4), 406–411 doi:10.1111/j.1365-2230.2008.02742.x. PubMed
Other websites
- Anthrax World Health Organization (WHO)
- CBRNE Anthrax Infection – Medscape Reference
- Images of anthrax on DOIA
