Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Dr Natalie Renaud, Registrar, and Dr Susan Bray, Sexual Health Physician, Sexual Health Clinic, Hamilton, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. September 2019.
Introduction
Demographics
Clinical features
Complications
Diagnosis
Treatment
Prevention
Genitourinary chlamydia infection, or chlamydiasis, is a sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis with its serotypes D–K. It is often just called 'chlamydia'.
C. trachomatis serotypes L1–L3 cause lymphogranuloma venereum, which is discussed separately.
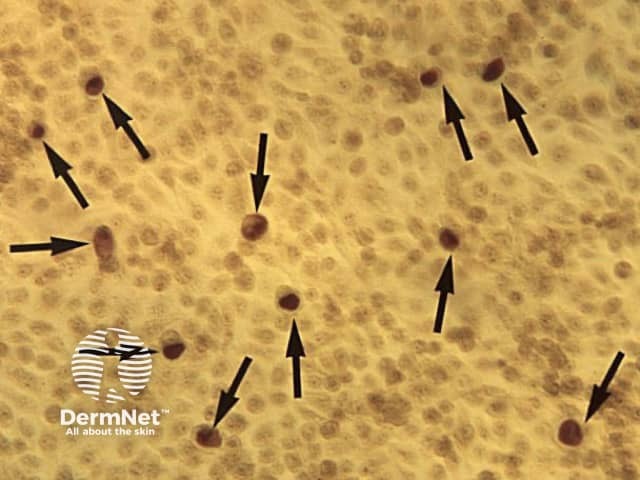
Chlamydia Geimsa Stain CDC2
Genitourinary chlamydia infection is a very common STI.
Risk factors include:
A genitourinary chlamydia infection may cause very mild symptoms or no symptoms at all; it is asymptomatic in approximately 70% of infected women and 50% of infected men.
In men, the most common signs and symptoms of genitourinary chlamydia infection are:
In women, the most common signs and symptoms of genitourinary chlamydia infection are:
Genitourinary chlamydia infection can lead to complications of variable severity and duration, particularly when following multiple infections over time.
The possible complications of genitourinary chlamydia infection in men include:
The possible complications of genitourinary chlamydia infection in women include:
Mother-to-child transmission can result in chlamydial conjunctivitis and pneumonia in newborn babies.
In symptomatic individuals with genitourinary chlamydia infection, examination findings may include urethral discharge, abnormal vaginal discharge, cervicitis (inflammation of the cervix) and contact bleeding, tenderness on bimanual examination (cervical excitation and pelvic adnexal tenderness), and rectal discharge. As these findings can also occur with other STIs, laboratory tests are required to confirm the diagnosis of chlamydia.
In men with suspected genitourinary chlamydia infection, clinical specimens may include:
In women with suspected genitourinary chlamydia infection, clinical specimens may include:
A urine sample is not routinely recommended in women because the bacterial load in urine is much less than in men.
Rectal and pharyngeal swabs can be taken by a clinician or the patient. A proctoscopy (examination of the rectum) should be performed if there are rectal symptoms suggestive of chlamydia infection.
Tests for genitourinary chlamydia infection may include:
Point-of-care testing using a NAAT or EIA is not routinely used. Chlamydia cultures are not widely available, have a low sensitivity (60–80%), and are not used for throat and rectal infections.
Individuals receiving treatment for genitourinary chlamydia infection should abstain from sex for at least 7 days.
Treatment for uncomplicated urogenital chlamydia infection includes:
Treatment for uncomplicated rectal chlamydia infection includes:
Doxycycline 100 mg twice daily for 7 days is used as a treatment for asymptomatic chlamydia infection at extra-genital sites.
Note that doxycycline is contraindicated in pregnancy and azithromycin is associated with QT prolongation.
Proctitis, epididymo-orchitis, and pelvic inflammatory disease due to chlamydia infection are treated by an extended course of empiric antimicrobial therapy while waiting for test results.
Treatment should cover other possible causes of these presentations such as gonorrhoea. Supportive measures and clinical review are required.
The management of chlamydia infection includes a full sexual health check to look for other STIs and the notification, treatment, and testing of sexual contacts.
If the patient is pregnant or has rectal chlamydia, a proof-of-cure test with a NAAT should be performed at least 4 weeks after the completion of treatment. If taken earlier, a false-positive result may occur due to remnant chlamydial DNA. Re-testing is recommended in 3 months as re-infection is extremely common.
As for other STIs, the risk of acquiring chlamydia infection is reduced by safe-sex practices, including limiting the number of sexual partners, using condoms, and avoiding re-infection by not having sexual contact with untreated sexual partners.
Postexposure doxycycline, taken within 72 hours of condomless intercourse, has been shown to reduce the incidence of chlamydia, syphilis, and gonorrhoea, in men who have sex with men by two thirds.
If you think you are infected, stop any sexual contact and see your usual doctor or a specialist clinician at a sexual health clinic.