Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Systemic diseases Diagnosis and testing
Author: Adjunct A/Prof Patrick Emanuel, Dermatopathologist, Clinica Ricardo Palma, Lima, Peru. DermNet Editor-in-chief: Adjunct A/Prof Amanda Oakley. August 2018.
Introduction Histology Special studies Differential diagnoses
Intralymphatic histiocytosis manifests as quite non-descript erythematous patches or plaques. Autoimmune disease (eg, rheumatoid arthritis), joint replacements, and malignancy, rosacea appear to be aetiologic factors.
In intralymphatic histiocytosis, the histopathology shows dilated lymphatic spaces stuffed with histiocytes and associated lymphocytes (figures 1,2,3). There is often oedema of the surrounding dermis. The overlying epidermis is uninvolved. In cases occurring around the eyes, it is common to find Demodex species in follicular structures (figure 4).
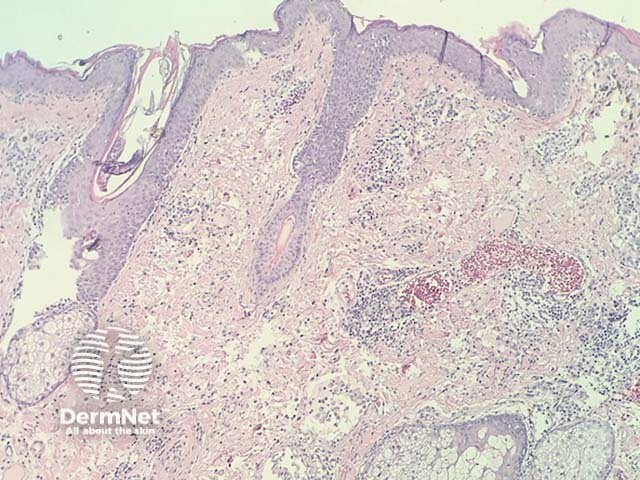
Figure 1
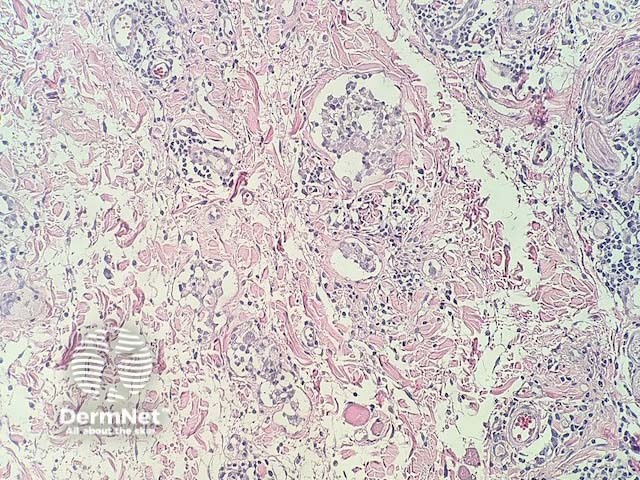
Figure 2
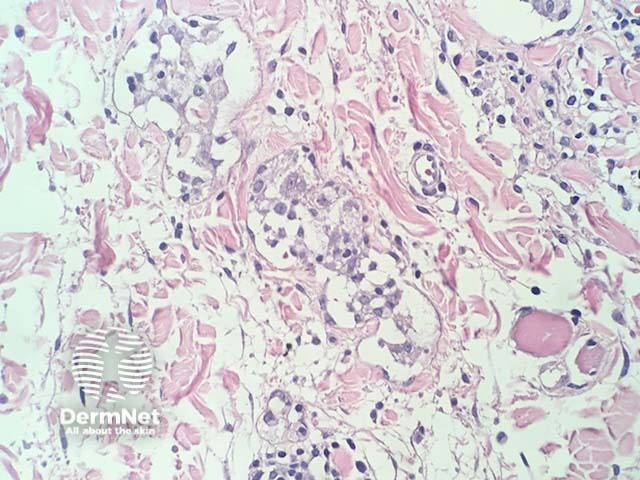
Figure 3
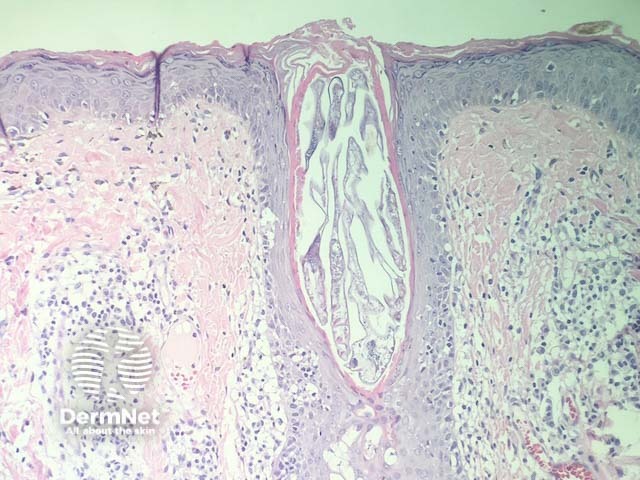
Figure 4
Immunohistochemical studies for lymphatics (eg, D2–40) highlight the lymphatic structures. Histiocyte markers (eg, CD68, CD143) highlight the histiocytes.
Emanuel PO, Lewis I, Gaskin B, Rosser P, Angelo N. Periocular intralymphatic histiocytosis or localized Melkersson-Rosenthal syndrome? J Cutan Pathol. 2015 Apr;42(4):289–94. doi: 10.1111/cup.12419. Epub 2015 Feb 3. PubMed PMID: 25370527. Journal