Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lesions (cancerous) Diagnosis and testing
This content was created by Miiskin — A proud sponsor of DermNet. April 2019.
Background Self-skin examination Skin Surveillance Offered to Address the Challenge of Catching Skin Changes Digital applications for Patient-Led Skin Monitoring Putting technology to good use High-Tech Technology to Empower Patient Monitoring Programmes Limitations of applications
Melanomas are notoriously difficult to discover and diagnose. After years of education through skin cancer awareness campaigns, patients or their close relatives are, nonetheless, often the ones to sound the early alarm about a concerning lesion. However, many patients are still surprised when the lesion they presented to the doctor, and in many cases another lesion, actually turn out to be a melanoma. The simple fact is that there is no typical appearance of a melanoma that is easily detected by the naked eye.
Melanoma survival rates are dramatically improved if a melanoma is detected early, especially when the malignant cells are confined to the tissue of origin — called melanoma in situ or level 1 melanoma. When melanomas are not caught early, and have invaded into the deeper layers of the skin, the survival rates drop.
For these reasons, it is recommended that any concerning lesion is presented to the appropriate physician as soon as possible. Many suspicious skin lesions that turn out to be melanomas are initially identified by the patient, so skin self-examination can contribute to early detection. It follows that encouraging effective skin self-examination is likely to assist in early detection of melanoma.

Patient consulting with a doctor
It is recommended that each person is to look out for changes to their skin’s appearance through skin self-examination. Changes in asymptomatic (atypical) moles and the appearance of any new lesions on the skin for those over 35 years of age are warning signs that should not be ignored.
Studies have shown that the average person may not be very proficient at skin self-examination, particularly when the change occurs over an extended period of time or in an area not easily seen. Patients and their partners may also not be very comfortable with being tasked to perform regular skin checks.
Unlike the pattern for the more prevalent carcinomas, the anatomical distribution of melanoma, albeit highly correlated, is also not only on skin exposed to UV rays, which makes the task more challenging. Even so, an extensive culture for full-body tanning in the summer – a culture that is still very prominent today – means that especially western populations have had extensive full-body exposure to UV light in their lifetime. Continued efforts to ban UV tanning beds and educate populations about sun protection are warranted, but perhaps not sufficient, and an increased focus on secondary prevention of skin cancer may also be needed.
Given the difficulties identified here, there is a concern that patients may not have sufficient awareness of their skin’s appearance and so may only catch any suspicious skin changes at a belated stage. Thorough total-body skin self-examinations, ideally assisted by a partner, should be more prevalent in consumers’ minds. Some campaigns have already been launched such as a campaign from the American Academy of Dermatology focusing on partner-assisted self-examinations.
The majority of melanocytic naevi (moles), spots, and bumps on the skin are harmless, but it is not always the case. As well as looking out for any “ugly duckling” that stands out from other moles, people are advised to look for changes in their existing moles and also be aware if any new spots appear within previously normal skin. In adults, 71% of nevus-associated melanoma show up as new lesions on the skin and not in existing moles, the need to also be aware of any new lesions is critical and may be quite unmanageable for patients with a large amount of nevi.

Digital dermoscopic photography
Given the need to closely inspect for changes to the skin, photographic skin surveillance, such as digital dermoscopy of individual lesions and full-body photography, have emerged and are now recommended. Many healthcare providers offer clinical photography for melanoma patients and some consumers also spend out-of-pocket on surveillance programs in private clinics. This is encouraging. The more skin that can be recorded with photography, the higher the likelihood of catching any future skin change at an early stage.
The Melanoma Institute Australia actively recommends the use of photos in the skin self-examination process: “The best way to monitor changes on your skin is by taking photographs every few months and comparing them to identify any changes. React quickly if you see something growing and/or changing”
However, there are a few challenges that should be addressed:
Some of these challenges are already addressed in some countries, such as New Zealand and Australia, where the problem of skin cancer is greatest. In other areas of the world, healthcare systems still need to address how best to meet the requirement and challenge of photographic surveillance of patients.
Applications for skin self-examination are being investigated and introduced as part of the solution. As well as providing reminders to perform regular skin self-exams, apps can have the following benefits:
Miiskin is one of the smartphone apps that facilitates thorough skin self-examinations. It does so by letting its users:
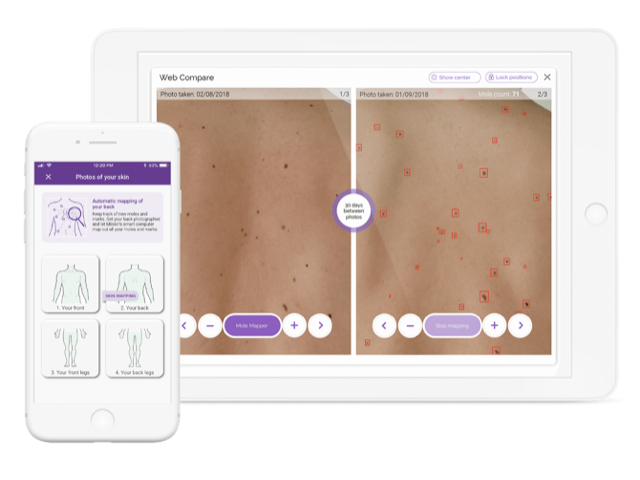
Miiskin Skin Mapping
The Skin Mapping solution is powered by an intelligent algorithm, which identifies the moles and marks on the skin that it can find, and so may help its user identify new moles or marks on the skin. It is not intended to take away the user’s responsibility for identifying changes to their skin. It is a way of making the experience more engaging for the user. Miiskin does not facilitate a diagnostic process — the focus is on the patient’s skin awareness and identification of skin changes.

Skin mole photo app
Miiskin is now the leading global skin surveillance app with over 300,000 downloads and has recently become the first app to receive independent dermatological accreditation from the Skin Health Alliance.
The Miiskin smartphone app is free for the basic version. The premium version of the app costs US$25 per year and it comes with a 30-day free trial for its users to try it out before they are charged anything. It can be downloaded from your smartphone application store (eg, Google Play, or App Store).
The Melanoma Risk Predictor, developed by Australian researchers (QIMR Berghofer Medical Research Institute), represents a useful way to take advantage of technology to help users understand their overall risk of melanoma. Note that the results cannot be guaranteed for non-Australians.
The Melanoma Risk Predictor can be accessed within the Miiskin app. As it is only available in English, it is currently available in the app to all English speaking countries.
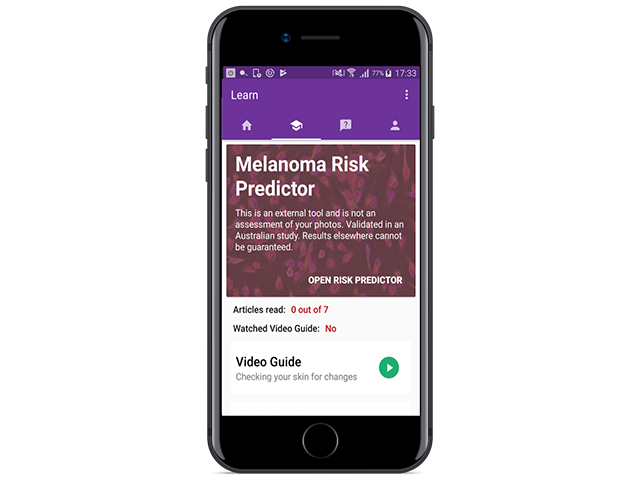
The Miiskin app features the Melanoma Risk Predictor
There is general evidence that smartphone apps such as Miiskin have been well received by users when implemented in health interventions in other areas.
A solution like Miiskin holds further potential for the future. An ever increasing number of healthcare providers are reaching out to hear how the smartphone application may be able to help their patients. In addition, patients enrolled in other photographic surveillance programs and clinical follow-up programs want to use Miiskin as an integrated part of their existing programme.
Some clinicians also advocate the benefits of physicians being able to view their patient’s Miiskin images together with the patient’s medical history. Efforts are being undertaken to investigate how such a teledermatological solution can safely be implemented in a clinical setting.
Other benefits of app technology may include:
If you are running a patient follow-up programme or are offering patient photographic surveillance, reach out to Miiskin on [email protected] to hear how Miiskin may integrate with, and help your programme.

Skin cancer prevention and detection leaflet
Miiskin are also offering free educational leaflets for those interested in educating their patients about secondary prevention of skin cancer. Request leaflets for your clinic here.
Home photo-monitoring of skin and moles should not replace a visit to the doctor.
Even though some research has shown promising results with algorithms for melanoma risk assessments of moles when pictures are taken in clinical contexts, there is still a long way to go before consumers can get a diagnosis or even an adequate automatic risk assessment through a smartphone.
The British Association of Dermatologists released a press release in July 2017 stating that apps aiming to detect or diagnose lesions based on smartphone photos should be treated with caution.
Teledermatology services have shown more promising results in real-life settings, and can be as good as an in-person examination by a specialist — when the total body examination and lesion selection is initially undertaken by a trained and experienced practitioner.