Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
Hair follicle staphylococcal infections include:
Surface infections tend to be itchy, deeper infections are more painful.
Boil Superficial bacterial folliculitis 




The differential diagnosis of superficial folliculitis includes:
Pseudomonas folliculitis is caused by inadequate chlorination of a hot tub or spa pool. Lesions cluster under the swimming costume. Spa pool folliculitis usually settles by itself, but severe cases can be treated with ciprofloxacin.
Pseudomonas folliculitis Pseudomonas folliculitis Pseudomonas folliculitis 


Malassezia or pityrosporum folliculitis is due to malassezia infection. It results in irritable monomorphic superficial papulopustules on the upper trunk. Managed with topical and/or systemic antifungal agents.
Pityrosporum folliculitis Pityrosporum folliculitis Pityrosporum folliculitis 


Acne is characterised by comedones, papules and pustules, sometimes with nodules, cysts and scars.
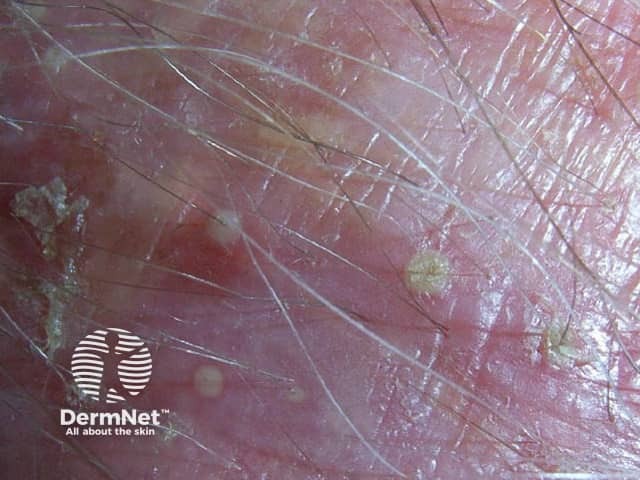
Irritant folliculitis is a rash due to shaving e.g. pseudofolliculitis barbae, waxing, or other form of epilation. Local keratolytics and if necessary oral tetracyclines can be helpful.
Pseudofolliculitis Pseudofolliculitis Pseudofolliculitis 


Chemical folliculitis arises in roadworkers (coal tar) and shearers (sheep's wool).
Shearer folliculitis 
Occlusive folliculitis arises because of excessive emollient use.
Keratosis pilaris is characterised by follicles plugged with keratin on upper arms and anterolateral thighs, sometimes erythematous.
Keratosis pilaris Keratosis pilaris Keratosis pilaris 


There are many other possible considerations. Non-follicular eruptions sometimes confused with folliculitis include:



Hidradenitis suppurativa is sometimes mistaken for boils. Hidradenitis affects the axillae, inguinal, perianal and submammary areas and results in inflamed boil-like nodules that may suppurate and scar. It does not respond to standard antibiotic therapy and S. aureus is infrequently cultured. Refer to a dermatologist for management.
Hidradenitis suppurativa Hidradenitis suppurativa 

Contributing irritants and occlusive emollients should be avoided where possible. Avoid plucking, shaving, waxing etc while infection is active and for several more weeks.
Staphylococcal infections are contagious, requiring careful attention to hygiene.
Localised staphylococcal infections may be managed using meticulous wound care (including incision and drainage of large furuncles and abscesses) and antiseptics as local application and cleanser. The routine use of topical antibiotics such as fusidic acid or mupirocin is undesirable because of increasing prevalence of topical antibiotic-specific and methicillin-resistant strains of staphylococci.
Oral antibiotics such as flucloxacillin or dicloxacillin may be prescribed for more extensive or recurrent infections but should not be prescribed for trivial reasons. Refer to a specialist if a course of several weeks does not prove helpful; some patients warrant additional treatment with rifampicin and clindamycin.
In recurrent cases, take swabs from active lesions and nostrils to determine antibiotic sensitivity. Consider predisposing causes:
Describe the evidence that vitamin c is of benefit for recurrent boils.
Information for patients
See the DermNet bookstore