Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
Malignant melanoma may arise from melanocytes found on the skin or rarely from mucosal surfaces, under the nails and in the meninges.
Melanoma may arise from common acquired naevi or from dysplastic naevi. They may also arise from the solar lentigo or atypical lentigo. Most arise de novo. The dermoscopic features are enormously variable. Early melanoma is relatively organised but as time progresses, it becomes more disorganised, and this is reflected by the dermoscopy.
Melanomas have features indicating their melanocytic origin:
Many other features have been described in melanoma. And they may be relatively featureless.
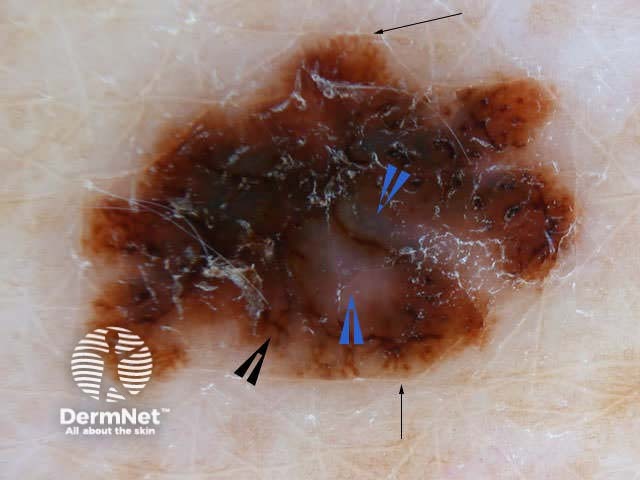
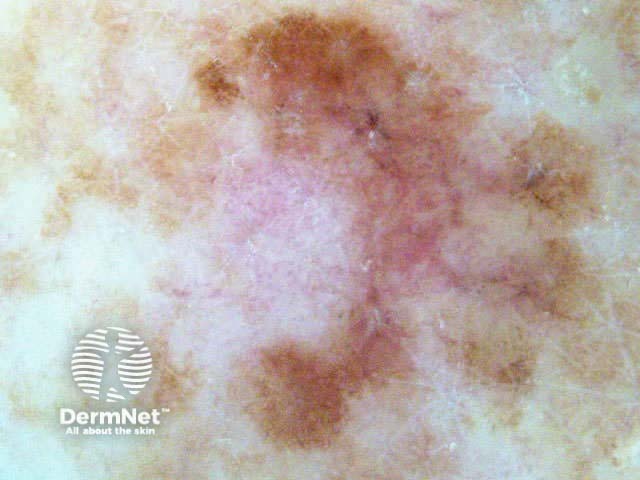
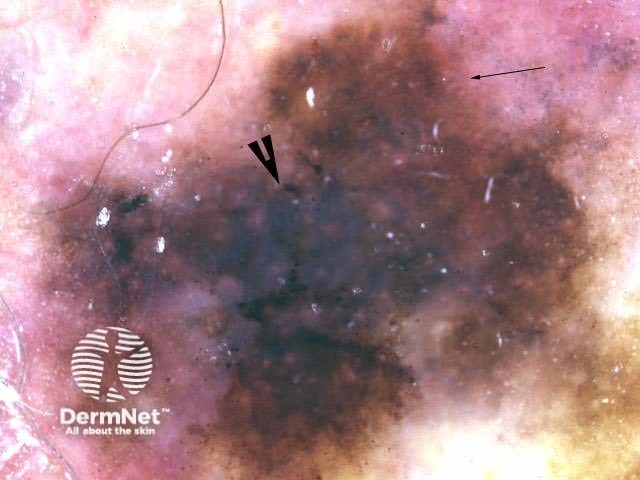
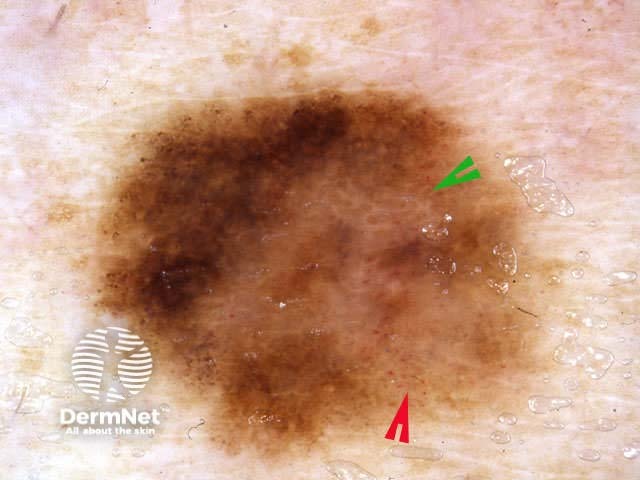
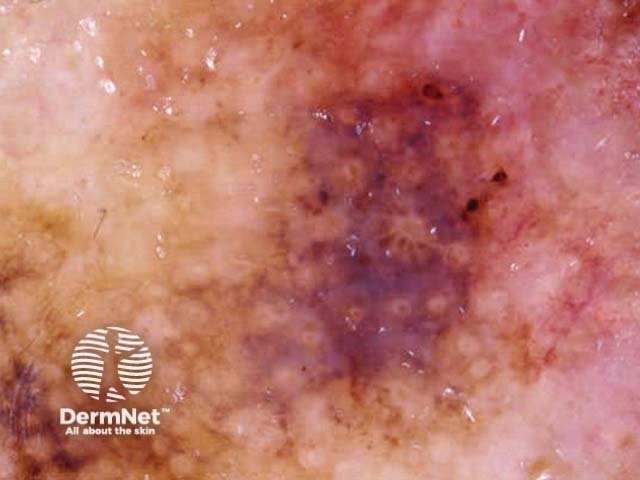
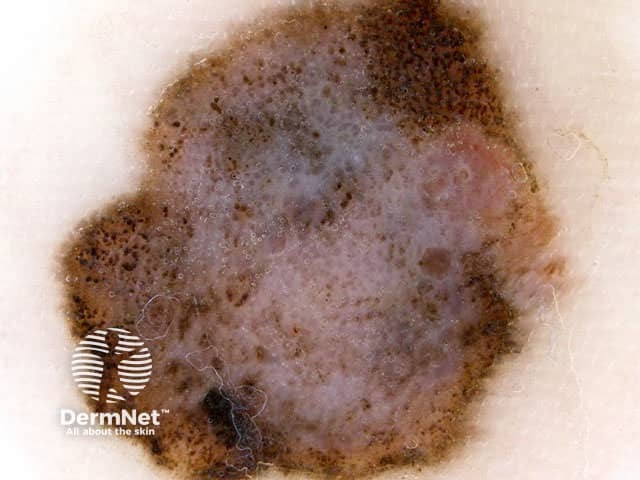
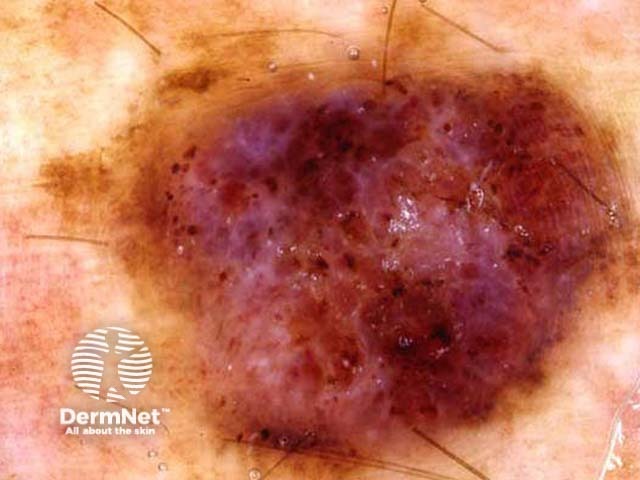
By the time in situ and invasive superficial spreading melanoma (SSM) is recognised as a changing or distinctive lesion by the patient or their doctor, it is often large (>6mm). Characteristically, superficial melanoma is asymmetrical and irregular in shape and structure.
Superficial melanomas usually have one or more of the following dermoscopic features:
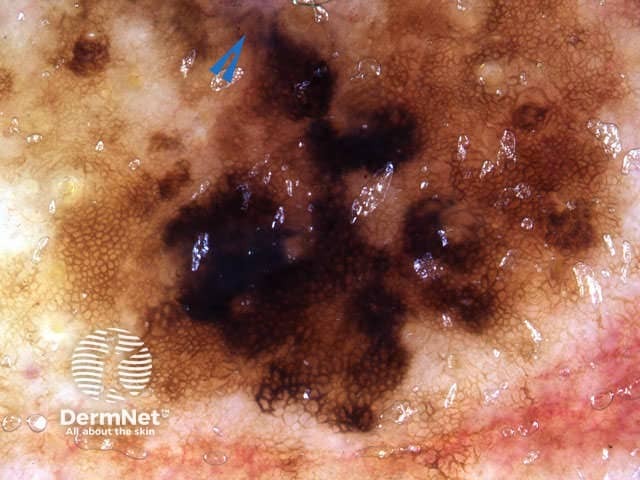
The blue-white veil is described as an irregular structureless area of confluent blue pigment with a ground glass haze, as if the image were out of focus. It is due to hyperkeratinisation over dense epidermal pigment. Uniform blue-white structures may be observed over some blue naevi and haemangiomas but in melanoma they are focal, asymmetrical and irregular.
Scar-like depigmentation due to regression of melanoma results in irregular white areas that must be distinguished from the uniform peripheral loss of pigment seen in benign halo naevi. It arises in about 50% of melanomas.
Negative network, although a feature of melanoma, may also be found in some benign melanocytic lesions (especially Spitz naevus) and seborrhoeic keratoses.
Some of the structural features may be subtle in early melanoma, as in several examples shown here. Melanoma may be recognised when there are only 2-3 colours in the lesion on dermoscopy (or 1-2 clinically). Deeper melanomas reveal more colours.
Irregular structure Irregular structure Irregular shape/structure Blue-white veil Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular structure Irregular shape/structure Irregular structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular structure Irregular structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure Irregular shape/structure 















The Breslow thickness, which measures the thickness of invasion, is measured in millimetres and is the most important prognostic factor.
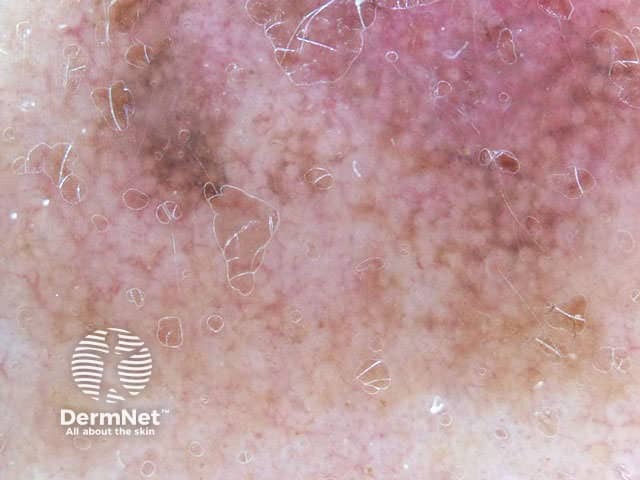
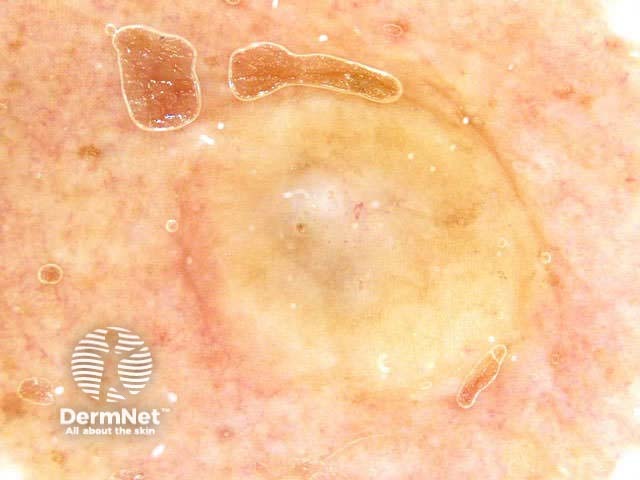
Lentigo maligna is a special type of melanoma in situ arising on sun damaged sites. The dermoscopic features of lentigo maligna are characterised by:
Lentigo maligna
Annular granular pattern and rhomboids seen in dermoscopy of lentigo maligna
Annular granular pattern seen in dermoscopy of lentigo maligna

Lentigo maligna
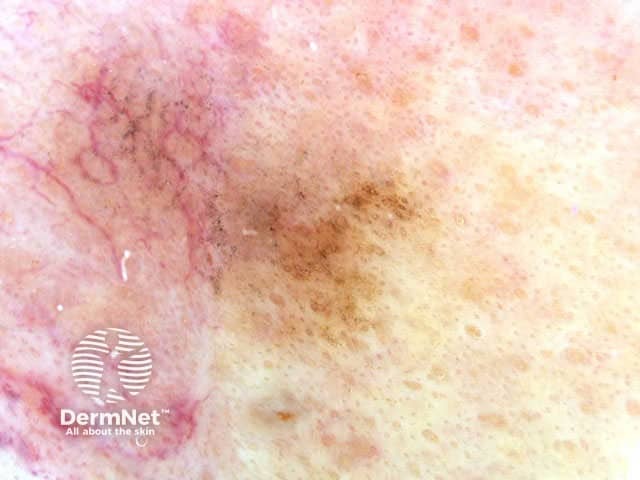
Lentigo maligna

Lentigo maligna

Lentigo maligna

Lentigo maligna
Lentigo maligna melanoma (invasive melanoma arising in lentigo maligna) shows the features of lentigo maligna in its in situ component, as well as features typical of invasive melanoma.
Irregular shape/structure
Irregular shape/structure

Irregular shape/structure
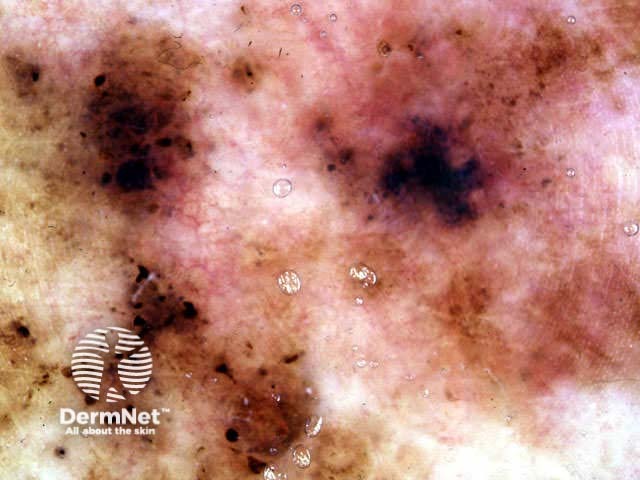
Not all facial melanoma have these characteristics. In the absence of network, there may be amelanotic areas and irregular blotches.

Melanoma

Irregular shape/structure
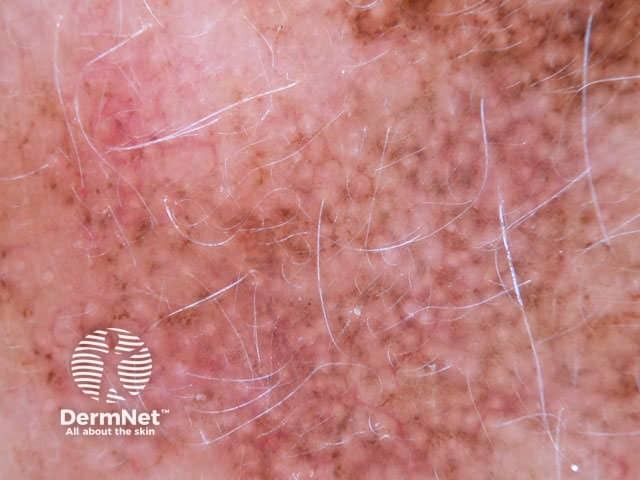
Lentiginous melanoma arises on the trunk and proximal limbs. It is usually diagnosed in the in-situ phase, and most often affects middle-aged and elderly men that have frequently exposed their backs to the sun. There is some argument regarding this entity and whether it can be distinguished from non-malignant atypical junctional hyperplasia or atypical junctional naevus in the elderly. Dermatoscopy may show features of solar lentigo, melanoma in situ and/or superficial spreading melanoma.

Lentiginous melanoma

Lentiginous melanoma

Lentiginous melanoma

Lentiginous melanoma
Compared with lentiginous melanoma, atypical junctional or lentiginous naevus is less atypical and asymmetrical in structure, and does not include polygons or grey structures. But some clinicians and pathologists believe these lesions are just on a spectrum of atypia, and these lesions often have marked asymmetry of structure on dermatoscopy.

Lentiginous naevus

Lentiginous naevus

Lentiginous naevus

Lentiginous naevus
This type of superficial spreading melanoma has large intraepidermal nests of tumour cells. These result in a globular pattern. The glbules are varied in shape, colour and distribution within the lesion.
Acral melanoma (palms and soles) tends to be much deeper than is suspected from its flat nature. Dermoscopically, it is characterised by a broad parallel ridge pattern rather than the benign parallel furrow pattern. The asymmetry and other features of superficial melanoma may be present.
Little white dots on the ridges are sweat ducts (acrosyringia) and confirm palmoplantar location. In melanoma, these dots disappear because the acrosyringia are destroyed by the malignant process.

Irregular structure

Irregular structure
Irregular structure
Subungual melanoma is a type of acral melanoma. Early lesions may show widening pigmented bands, irregular in spacing and varying colour (including pink or red in amelanotic melanoma). A positive Hutchinson's sign refers to pigment arising on the skin adjacent to the nail, which is rare in benign naevi. Changes may be observed by dermoscopy before they are evident clinically. Single pigmented bands should be followed by dermoscopy after several months.

Melanoma

Melanoma

Melanoma

Melanoma
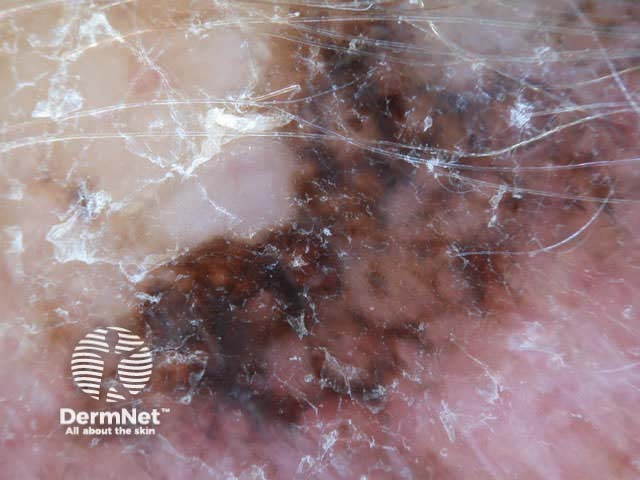
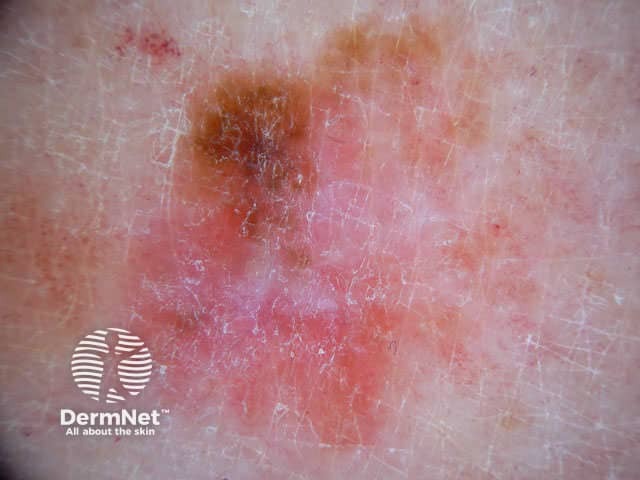
Nodular melanoma is often difficult to identify clinically. It can also be missed by dermoscopy if melanoma features are not noted on the periphery of the lesion. The lesion may composed of only two or three colours and these may be distributed fairly symmetrically. Sixty percent of nodular melanoma is amelanotic. Features often include:
Nodular lesions with suspicious features should be excised rather than followed up – delay may be dangerous. They may resemble seborrhoeic keratosis, basal cell carcinoma or angioma.

Irregular structure

Irregular structure
Irregular structure

Irregular structure

Irregular structure

Irregular shape/structure

Irregular shape/structure

Regular shape
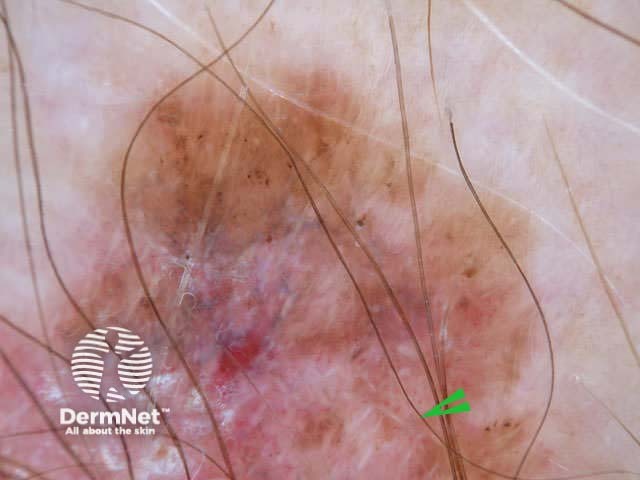
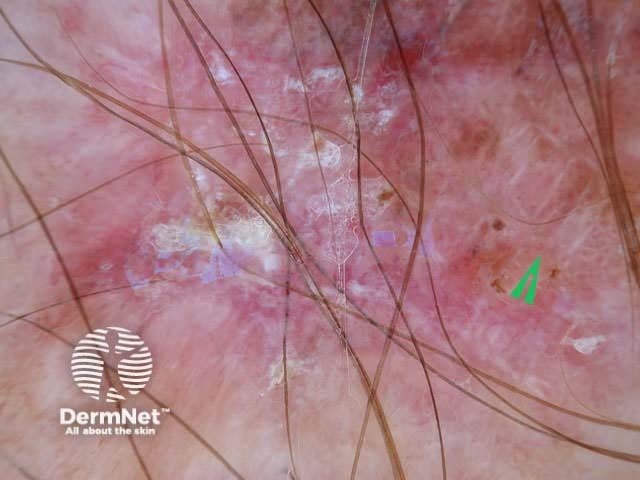
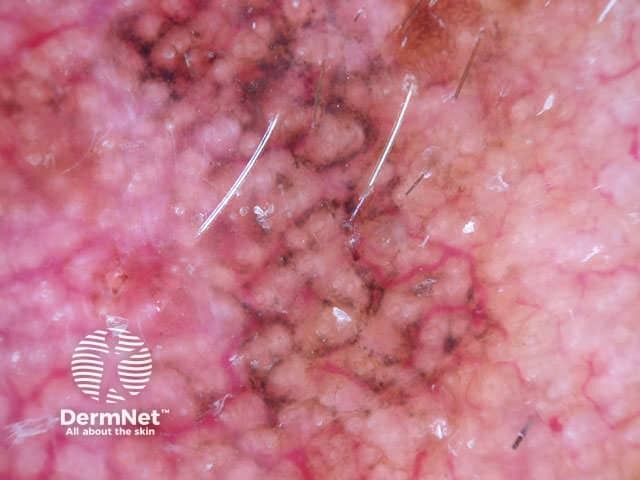
Amelanotic melanoma can be difficult to diagnose by dermoscopy. It should be considered if there is history of change within an odd-looking pink lesion. There is nearly always a small amount of focal and irregular pigmentation, often on the periphery of the lesion. Atypical vascularity may be a clue, with linear, dotted, corkscrew or polymorphous vessels. Too much pressure by the dermoscopy instrument may obscure the vascular pattern.

Melanoma

Amelanotic melanoma dermoscopy

Melanoma
Melanoma
Amelanotic melanoma dermoscopy
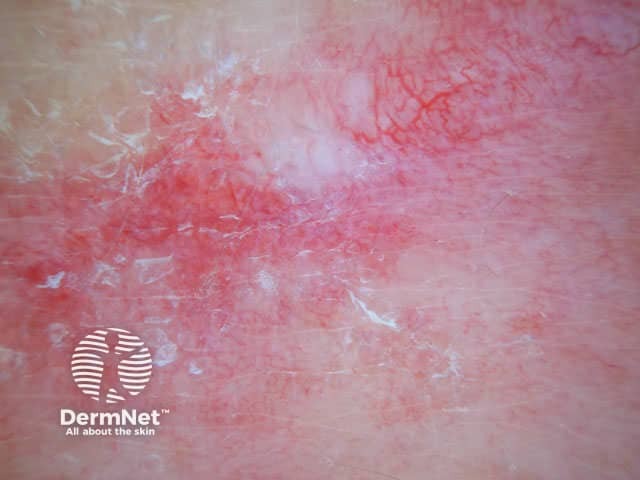
Amelanotic melanoma dermoscopy

Melanoma

Melanoma
Dermoscopic structures in desmoplastic melanoma may include atypical vascular structures, grey dots, or other melanoma-specific structures. When associated with lentigo maligna, features of lentigo maligna may coexist. This form of melanoma may be difficult to differentiate from dermatofibroma, clinically and on dermatoscopy.
Desmoplastic melanoma 1, dermoscopy 
How do dermoscopic features of melanoma vary with increasing Breslow thickness?