Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Palmoplantar and nail psoriasis
Created 2009.
Learning objectives
- Identify and manage palmoplantar and nail psoriasis
Note. You should have already read the overview page about psoriasis.
Clinical features of psoriasis
Psoriasis affecting the dorsal or ventral surfaces of the hands and feet may resemble psoriasis in other sites, with well demarcated erythematous scaly plaques. Fissuring can be troublesome.
Chronic plaques of psoriasis Chronic plaques of psoriasis Chronic plaques of psoriasis 


There are also distinct subtypes of palmoplantar psoriasis.
Palmoplantar keratoderma
Keratoderma refers to chronically thickened palms and soles and may be due to various inherited keratin gene disorders and acquired diseases. Psoriatic keratoderma is recognised by:
- Well demarcated erythema, surface scaling and fissuring of variable degree
- Limited in extent or affecting entire palms and soles
- Isolated finding or associated with typical plaques of psoriasis elsewhere
Keratoderma Keratoderma Keratoderma 


Nail psoriasis
Nails may be the only site affected by psoriasis and is frequently mistaken for onychomycosis (fungal infection), with which it may coexist. It is particularly common in those with psoriatic arthritis affecting the digits. It is usually asymptomatic but may be painful. It is very persistent and resistant to treatment, because it takes a year or so for new cells produced at the matrix to reach the distal edge of the nail plate. Signs affecting one or more nails may include:
- Pitting
- Onycholysis and nail bed erythema (oil-sign)
- Subungual hyperkeratosis
- Ridging and thick hard discoloured nail plate
- Complete destruction of the nail
Nail psoriasis Nail psoriasis Nail psoriasis Nail psoriasis Nail psoriasis Nail psoriasis 





The nail psoriasis index was devised to evaluate the signs of nail psoriasis in each nail separately, each on a 1-3 scale: pitting, Beau's lines, subungual hyperkeratosis and onycholysis in the matrix, the subungual tissues distal to the lunula, or the whole nail unit.
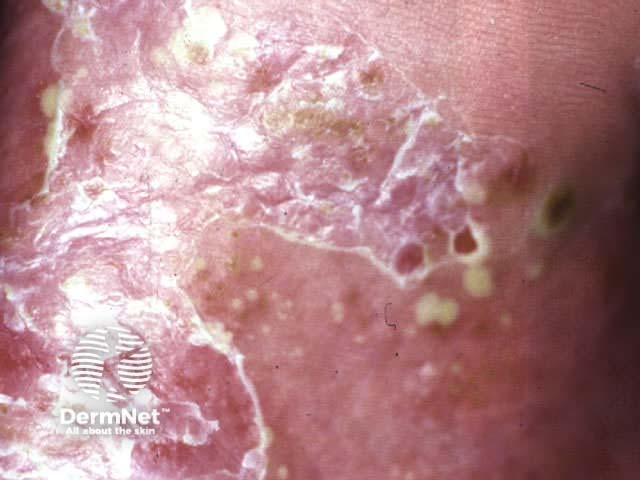
Localised pustular psoriasis
Localised pustular psoriasis affects one or both palms and/or feet. When it arises in the absence of psoriasis elsewhere, it may be called ‘palmoplantar pustulosis’.
- Chronic eruption of pustules on erythematous base on the palms and/or soles
- Nearly all patients are smokers or ex-smokers
- Very persistent and often resistant to treatment
Localised pustular psoriasis Localised pustular psoriasis Localised pustular psoriasis 

Acrodermatitis continua of Hallopeau
Acrodermatitis continua of Hallopeau is a chronic recurrent pustulation of nail folds, nail bed and distal fingers leading to loss of nails. it may occur alone or in association with chronic plaque psoriasis, psoriatic arthropathy, palmoplantar pustulosis and/or generalised pustular psoriasis.
Acrodermatitis continua 
Differential diagnosis
Palmoplantar psoriasis may be confused with:
- Hand dermatitis (more itch, vesicles, patchy dryness rather than keratoderma)
- Tinea manuum (elevated border, slowly extending edge, positive mycology)
- Other forms of keratoderma
Localised pustular psoriasis may be confused with:
- Pompholyx (clear vesicles instead of pustules): psoriasis may coexist
- Tinea manuum/pedis (asymmetrical, positive microscopy)
- Bacterid (pustules in response to systemic bacterial infection)
- Herpetic infection (unilateral, grouped, painful, umbilicated vesicles)
- Pustulosis acuta generalisata (rare pustular disorder of unknown cause)
Investigations
Investigations indicated in palmoplantar psoriasis may include:
- Skin swabs for bacteriology: to identify secondary infection (Staph. aureus and Strept. pyogenes)
- Scrapings and nail clippings for mycology: dermatophyte infection may co-exist with psoriasis
Management
Mild palmoplantar plaque psoriasis is usually managed with topical agents.
- Calcipotriol ointment (take care not to touch face)
- Ultrapotent topical steroids intermittently e.g. pulse therapy at weekends
- Thick emollient barrier creams
Keratoderma is unresponsive to topical steroids and calipotriol. Use emollients that incorporate keratolytic agents such as 5% salicylic acid or up to 40% urea (e.g. heel balm).
Nail psoriasis is very refractory to treatment. Very patient subjects may see results from calcipotriol or fluororuacil solution applied to nail folds and hyponychium twice daily for at least 12 months. Injected triamcinolone acetonide is rarely used because of pain and the potential to cause atrophy. Systemic therapy may be helpful but is rarely warranted for nail disease in the absence of troublesome psoriasis elsewhere.
Palmoplantar pustulosis is usually initially managed with intermittent ultrapotent topical steroids (continuous treatment aggravates the condition), crude coal tar ointment, and/or emollients.
If palmoplantar psoriasis is severe and interferes with function (painful to walk or work), refer to a dermatologist. Do not prescribe oral corticosteroids as these often make the condition worse and more difficult to control by other means. Possible treatments include:
- Bath photochemotherapy (PUVA soaks) or other forms of phototherapy
- Acitretin
- Methotrexate
- Ciclosporin
- Dapsone
- Colchicine
Activity
Provide advice about footwear for a patient with plantar psoriasis.
References:
On DermNet:
Information for patients
Other websites:
- Medscape Reference:
- Merck Manual Professional: Psoriasis
Books about skin diseases:
See the DermNet bookstore
