Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Dr Gia Toan Tang; A/Prof Rosemary L Nixon, Occupational Dermatology Research and Education Centre, Skin Health Institute, Melbourne, VIC, Australia. Medical Editor: Dr Helen Gordon, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. September 2020.
Introduction
Features specific to children
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Allergic contact dermatitis is a delayed type hypersensitivity reaction in the skin following skin contact with an allergen [1].
Allergic contact dermatitis is common in children because their skin can be easily sensitised. Compared to adults:
Sensitisation mainly occurs in newborns and infants aged 0–3 years, and the prevalence of subsequent allergic contact dermatitis increases with age [1].



Common allergens that trigger allergic contact dermatitis in children include:
The relevant allergens in children vary with age. For example, allergic contact dermatitis caused by nickel is more common in adolescents than in newborns, as older children acquire piercings and wear jewellery and belts [3].
The clinical presentation of allergic contact dermatitis in children is similar to that in adults.
Rare morphologies, such as erythema multiforme, pigmented purpuric eruption, and pustular or granulomatous reaction patterns, are unlikely to occur in children because exposure to the allergens associated with these particular presentations is unlikely (eg, tropical woods, rubber diving suits) [4].
Allergic contact dermatitis in children can spread to cause a generalised rash (autoeczematisation) [5].
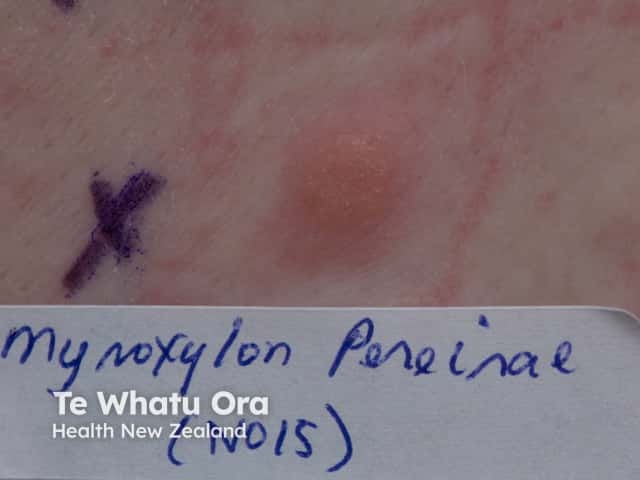
Systemic contact dermatitis is rare in children, with the most likely culprit being Myroxylon pereirae in food flavouring agents.
Allergic contact dermatitis is suspected clinically and is confirmed by patch testing. Patches containing the test substances are applied to the back for 48 hours, and the tests are assessed 48–96 hours later to identify the culprit allergen(s) [6]. In 2018, the first Paediatric Baseline Series was developed in the United States. Following this, the Australian Paediatric Baseline Series of 30 allergens was proposed, as compared to the larger Australian Baseline Series (for adults) of 60 allergens. [2].
Patch testing in children has a reasonable positive predictive value [2,7]. However, there may be false positives and false negatives [7,8]. It can be difficult to discriminate between irritation caused by the tested substances and weak allergic positive patch tests [7].

False positive patch tests

As in adults, other conditions that can look similar to allergic contact dermatitis should be considered in children. These can include the following.
The most important aspect of management is to identify the causative allergen. This may be obvious from the history or it may be necessary to perform patch testing.
Treatments, including emollients, should contain as few allergens as possible, since preservatives are a common cause of allergic contact dermatitis [5,6].
Allergic contact dermatitis has been reported to result in psychological effects in carers as well as in the affected child, inducing anxiety and depression. Therefore, psychological support should also be considered [3].
Counselling regarding allergen avoidance strategies is essential.
As with adults, once sensitised, contact allergy may persist, so skin contact with culprit allergens should be avoided lifelong [4].