Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Last Reviewed: June, 2025
Author: Dr Aliana Corlett, Medical Registrar, Wellington Hospital, New Zealand (2025)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction
Mechanism of action
General uses
Uses in dermatology
Contraindications
Benefits
Side effects and risks
Supply issues
Glucagon-like peptide 1 (GLP-1) is an incretin hormone that plays a central role in glucose homeostasis. GLP-1’s primary function is to stimulate glucagon dependent release of insulin from the pancreas. GLP-1 agonists reproduce and enhance the effects of natural GLP-1. These effects include decreasing blood glucose, reducing inflammation, reducing gastric emptying, and increasing satiety. Activation of GLP-1 pathways are being recognized as decreasing the inflammatory response in various organ systems where their receptors are expressed and carrying out protective and regulatory functions.
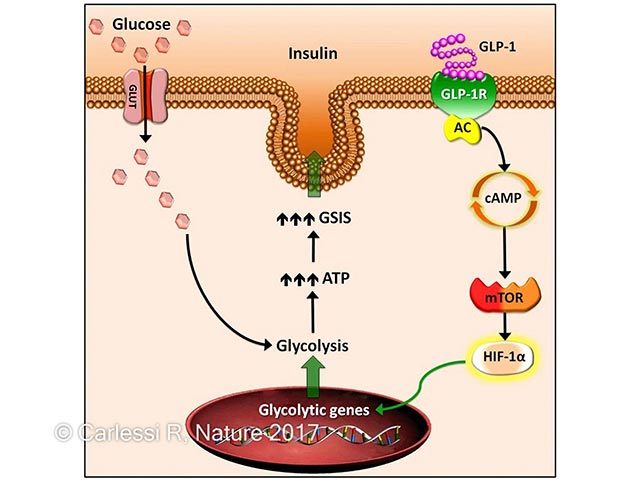
The mechanism by which GLP-1 promotes glucose dependent insulin secretion from pancreatic B cells is as follows. The normal response to carbohydrate ingestion is a rise in blood glucose and increased B cell glucose metabolism. However in type 2 diabetes, B cell glucose metabolism is dysfunctional, resulting in elevated blood glucose levels.
GLP-1 agonists bind to GLP-1 receptors on the surface of B cells, leading to an increase of cAMP. cAMP activates protein kinase A and Epac2 which act to increase insulin secretion.
Chronic stimulation of the GLP-1 receptor also increases glycolysis and ATP production in B cells via upregulation of glycolytic enzymes.
The mechanism of GLP-1’s anti-inflammatory action is still being studied, however its action has been demonstrated to involve regulating lymphocyte proliferation, maintaining regulatory peripheral T cells.
Most commonly known by their brand names, Trulicity (dulaglutide), Ozempic and Wegovy (semaglutide) and Saxenda and Victoza (liraglutide), GLP-1 agonists have been approved for use in management of type two diabetes and for weight loss. The medication is associated with an approximate 15% reduction in weight after 1-2 years. Most of the weight loss occurs within the first 6 months of use, and this weight loss is associated with improvements in blood glucose control, blood pressure management and triglyceride levels.

Dulaglutide (brand name Trulicity), one of the GLP-1 agonists used in diabetes management
As of 2024, GLP-1 agonists have not received FDA approval for dermatological uses such as psoriasis, hidradenitis suppurativa, or wound healing. Though case studies have demonstrated improvement in these conditions, further research and clinical trials are required before receiving approval.
Case studies have demonstrated improvement of the following conditions with the GLP-1 agonists listed.

Chronic plaque psoriasis in a lady with a BMI of 34
Conditions, such as psoriasis, are associated with excess secretion of proinflammatory cytokines and upregulation of GLP-1 receptors. The use of GLP-1 agonists is associated with an improvement of psoriasis symptoms due to its immunomodulatory effect. These are thought to be related to a reduction of dermal T cells and interleukin-17 expression. GLP-1 downregulates the inflammatory process through reducing expression of cytokines induced by TNF-a. A randomised, double blinded controlled trial is underway in Bosnia and Herzegovina expected to be completed at the end of 2024. A meta-analysis completed in 2021 including 4 controlled trials demonstrated that liraglutide therapy could improve psoriasis in type 2 diabetic patients independently of changes in weight and glycaemic control.

Axillary hidradenitis in an obese individual
This cutaneous inflammatory disease shares immunopathogenic pathways with psoriasis. In hidradenitis suppurativa (HS), there appears to be a dysregulated adipokine release that is shifted towards pro-inflammatory adipokines. The first case study of successful treatment of HS with a GLP-1 agonist, liraglutide was published in 2017. A 2023 case study demonstrates successful treatment of HS using long acting semaglutide, with a 24 kg weight loss and no further HS flares after 6 months. Systematic studies are limited and there are no active clinical trials investigating the effects of GLP-1 agonists on this condition. Insulin resistance is known to be a key player in the development of HS, hence further research into the effects of GLP-1 agonists is needed as they stimulate glucose dependent insulin secretion.
Through their activation of the cAMP-PKA pathway, they protect against oxidative stress and interfere with signalling of receptors for advanced glycation end products. GLP-1 agonists encourage wound healing through increasing the activity of tissue inhibitors of matrix metalloproteinases (TIMPs), slowing down degradation of extracellular matrix proteins.
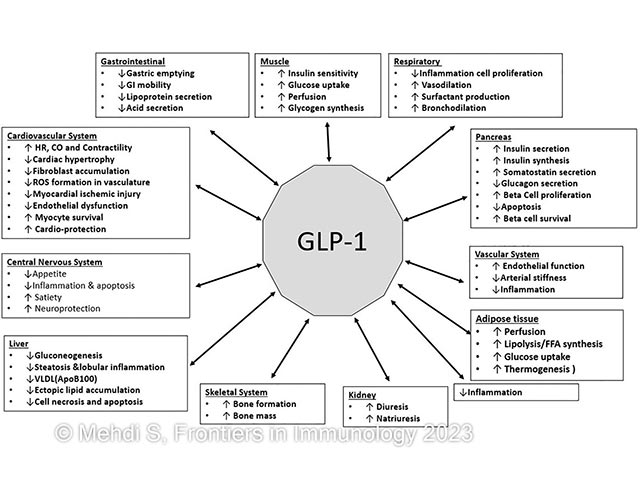
The image below demonstrates the effects of GLP-1 agonists on various systems:
The most common adverse drug reactions reported with GLP-1 agonists are as follows:
These include:
In New Zealand, dulaglutide (Trulicity) was the first approved GLP-1 agonist, made available for the treatment of Type 2 Diabetes in 2021. Though it is fully funded with special authority approval, supply issues mean it has become inaccessible to many despite increased demand. Hence, Pharmac temporarily funded liraglutide (Victoza) from March 1, 2023.
From May 1 2024, NZ funding for dulaglutide and liraglutide was limited to people already taking the medications due to a global supply shortage. This supply issue has been present since September 2022.