Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Hon A/Prof Amanda Oakley, Dermatologist, 1997; Updated: Dr Harriet Bell, Medical Registrar, New Zealand, May 2022. Minor update by Ian Coulson, Dermatologist. Copy edited by Gus Mitchell. July 2024
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outcome
Alopecia areata is an autoimmune condition affecting hair follicles causing hair loss. It typically presents with discrete bald patches on the scalp but can cause hair loss from all hair-bearing areas on the body.
Alopecia is a Latin term meaning hair loss, and areata refers to the patchy nature of the hair loss. The term alopecia areata is considered an umbrella term, which encompasses a number of variants including alopecia areata totalis or universalis, ophiasis, ophiasis inversus, and diffuse alopecia areata.

A single patch of alopecia areata (AA-patient1)

Extensive patchy alopecia areata

Alopecia totalis

Ophiasic pattern alopecia areata (AA-patient5)

Extensive alopecia areata with retention of grey hairs
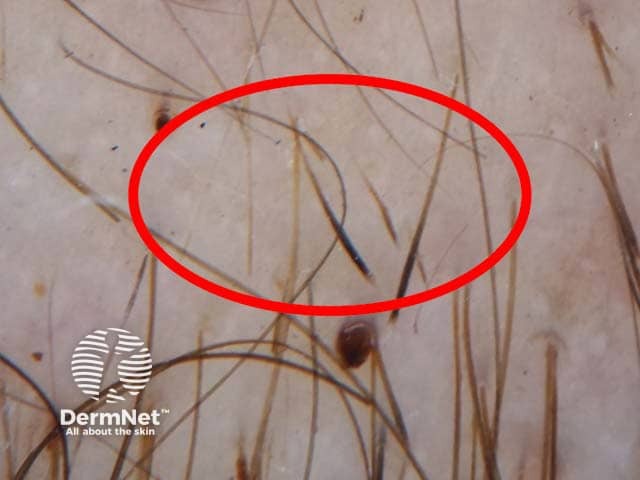
Dermoscopic image of alopecia areata presenting with exclamation mark hairs
The lifetime risk of alopecia areata is approximately 2%. It affects children and adults of all skin and hair colours. Peak incidence occurs in the second and third decades and most patients experience onset before the fourth decade. Alopecia areata does not carry significant sex or ethnic predominance.
The following may increase the risk of alopecia areata:
A normal hair follicle cycles through multiple phases:
The exact mechanism responsible for hair loss in alopecia areata remains unclear. It is hypothesised that loss of immune privilege in anagen hair follicles plays a key role in the pathogenesis, and genetic susceptibility is also thought to contribute.
This hypothesis is supported by the observation of a dense perifollicular infiltrate of T cells on histopathological examination of anagen follicles in alopecia areata; an area that is normally sparse of immune cells.
Acute onset of hair loss may manifest in a number of patterns.
Patchy alopecia areata is the most common pattern, producing:
The scalp is most commonly affected, but may also affect the:
Less common patterns include:
Characteristic “exclamation point hairs” may be observed, particularly at the periphery of bald patches. An exclamation point hair is a broken strand with a relatively thick distal portion and thin proximal portion as it enters the scalp. They are the result of anagen arrest and cessation of hair shaft formation, with weakening and tapering of the shaft.
Some patients may experience localised tingling or itching preceding hair loss (trichodynia).
Upon regrowth, hairs may initially lack pigment and so grow back as white or blonde.
Nail changes can be seen in an estimated 10–40% of patients and tend to be associated with more severe disease.
There are no differences in clinical features of alopecia in patients with skin of colour.
Alopecia areata is typically diagnosed on clinical features, however additional tests may aid diagnosis.
Scalp alopecia areata is assessed on the basis of the percentage of the scalp that is affected - this is the SALT score.
SALT 0 means there is not hair loss due to alopecia areata.
SALT 50 means 50% of the scalp is affected by alopecia areata. SALT 40 is regarded by sufferers and dermatologists as severe alopecia areata.
Lash and brow alopecia can be difficult to disguise and adds to the burden of the condition.
The ASAMI score (Alopecia Areata Severity and Morbidity Index) has recently been devised to take into account not only sites and extent of alopecia, but sufferer centred symptoms such as difficulty in camouflage, affects on work recreation, relationships, and mental wellbeing.
There is no cure for alopecia areata. The hair loss in alopecia areata is associated with minimal harmful physical effects and spontaneous resolution may occur.
However, the psychological impact can be significant, therefore warranting treatment. Numerous therapies have been used with variable response and high quality evidence is lacking.
Intralesional corticosteroid injections
Topical treatments
Topical immunotherapy
Others
Improvement following numerous other less common and less studied treatments have been reported.
Patients should be informed that there is no cure and response to treatments are variable.
Camouflaging hair loss can be helpful for patients who decide against pharmacological treatment or in those who have incomplete response.
A prosthesis can be used to disguise scalp hair loss.
Styling products such as gels, mousses, powders, and sprays help to keep hair in place, achieve scalp coverage, and add volume.
False eyelashes or artificial eyebrows
We do not yet know how to prevent alopecia areata.
Alopecia areata follows an unpredictable course. Spontaneous hair regrowth and recovery may occur and is common in some reports. Relapse is also common, however, and patients may have several phases of hair loss and subsequent regrowth. The risk of progression to alopecia totalis or alopecia universalis is approximately 5–10%, from which recovery is unlikely.
Response to treatment is highly variable and hair loss may recur when therapy is stopped.
Poor prognostic factors include: