Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author(s): Dr Delwyn Dyall-Smith FACD, Dermatologist, Australia, 2011. Updated: Dr Naya T. Hassan, Dermatology Resident, Syria. Copy edited by Gus Mitchell. Updated May 2022
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Lichen planopilaris is an uncommon inflammatory condition that can lead to permanent hair loss.
The disease is considered to be a form of lichen planus which affects the hair follicles. It results in patchy, progressive, permanent hair loss mainly on the scalp, although other hair bearing skin (brows, pubic, and body) may be affected. Several forms are recognised:

Lichen planopilaris

The atrophic scalp of a male patient with Graham-Little syndrome (LPP-patient2)

Madarosis due to lichen planopilaris

Clinical image of Graham-Little syndrome, presenting with alopecia of the forearm (LPP-patient2)
The exact cause of lichen planopilaris is unknown. It is thought to be a cytotoxic autoimmune response to an unknown antigen located in hair follicles. The disease is rarely gene-related. It is also rarely drug-induced, eg, pembrolizumab.
Lichen planopilaris typically presents as smooth white patches of scalp hair loss. No hair follicle openings can be seen in the areas of hair loss. Scale and redness surround each hair follicle at the edges of these patches, which may be spiny on palpation. Hairs can be easily pulled out. It is multifocal and small areas may merge to form larger irregular areas.
Common sites of involvement are the sides, front, and lower back of the scalp.
Symptoms are often absent, but they may include:
Lichen planopilaris is usually slowly progressive.
Diffuse hair loss is uncommon.
The clinical features do not vary in differing skin types.
Lichen planopilaris is suspected on the clinical presentation and careful examination of the mouth, nails, and skin for evidence of lichen planus elsewhere.
Trichoscopy reveals absent follicles, white dots, tubular perifollicular scale, and perifollicular erythema.
The diagnosis may be confirmed on scalp biopsy that includes hairs with surrounding redness and scale at the edge of an area of hair loss. Lichen planopilaris is an example of a primary lymphocytic folliculitis.
However, it is not always possible to make a diagnosis on biopsy. Where there is only patchy scarring, hair loss, and no evidence of inflammation, the diagnosis may not be able to be confirmed.

Dermoscopic image of lichen planopilaris presenting with irregularly distributed follicular openings (red arrows) denoting scarring (cicatricial) alopecia
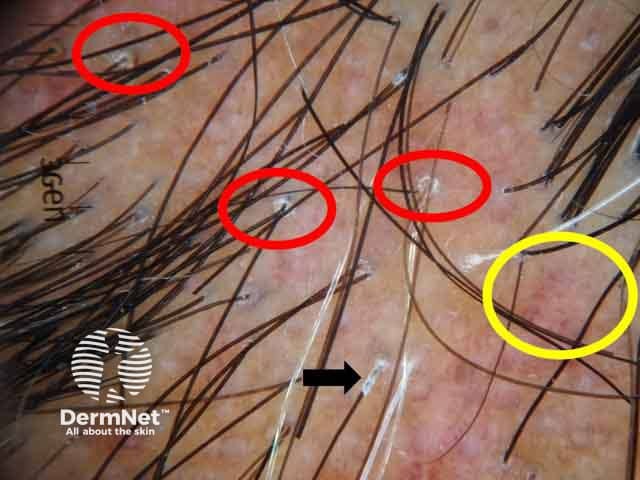
Dermoscopic image showing perifollicular scales (red circles, peritubular cast (black arrows) and blue grey dots (yellow circles) (LPP-patient1)
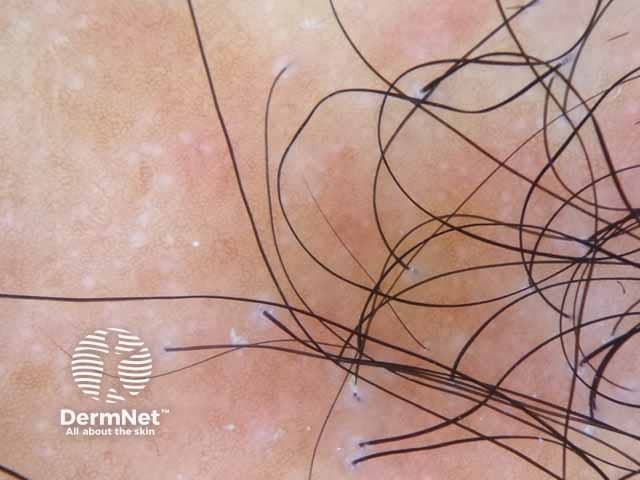
Dermoscopic image of Graham-Little syndrome showing perifollicular scales of the scalp lesion denoting lichen planopilaris (LPP-patient2)
Treatment should be sought and provided early, as no treatment restores hairs that have already been lost and replaced by scarring. The aim of treatment is to slow the progression of the disease and relieve symptoms. Hair loss may continue, although at a slower rate.
Anti-inflammatory treatment options include:
Response to treatment is variable and some published studies contradict others as to their efficacy. The best patients can expect is to stop the progression of hair loss and to minimise scalp discomfort.
A management protocol as suggested by Svigos et al. (2021) includes:
The prognosis of the disease cannot be predicted. It may improve on its own after a period of time, or can get progressively worse. The main goal of treatment is to stop the hair loss, but the response to treatment also varies amongst patients.