Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Laboratory tests for bacterial infections — extra information
Infections Diagnosis and testing
Laboratory tests for bacterial infections
Author: Natasha Lee BSc (Hons), Visiting Medical Student, University of Leeds. DermNet Editor-in-Chief: Hon A/Prof Amanda Oakley, Hamilton, New Zealand. August 2014.
Introduction
Skin samples
Bacteria culturing
Antibiotic sensitivity testing
Gram stain
Other bacterial culture tests
Blood tests
Polymerase chain reaction (PCR)
Enzyme-linked immunosorbent assay (ELISA)
Why do we need laboratory testing for bacterial infections?
Various tests are carried out in a laboratory to establish or confirm the diagnosis of a bacterial skin infection. Although a thorough history and examination of the patient are vital, laboratory tests can help the clinician to reach a diagnosis.
The culture of the bacterial species with antibiotic sensitivity testing is considered the gold standard laboratory test.
Skin samples for bacterial testing
Skin samples can be collected in the following ways.
- A dry sterile cotton-tip swab is rubbed on the suspicious skin site, for example, blistered or dry skin lesions or pustules.
- A moist swab is taken from a mucosal surface, such as inside the mouth.
- Aspiration of fluid/pus from a skin lesion using a needle and syringe (this is more likely than a swab to yield the organism)
- A skin biopsy: a small sample of skin removed under local anaesthetic.
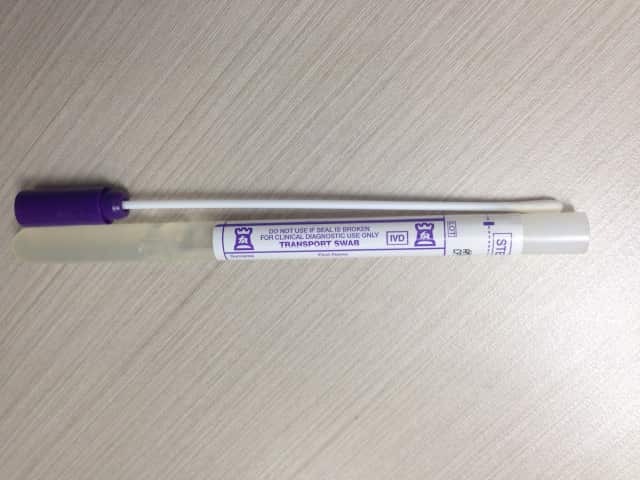
Bacterial skin swab
What is meant by culturing bacteria?
Culturing or growing bacteria is most commonly done by brushing the skin swab on sheep blood agar plates and exposing them to different conditions. Which bacteria grow depend on the medium used to culture the specimen, the temperature for incubation, and the amount of oxygen available.
- An obligate aerobe can only grow in the presence of oxygen.
- An obligate anaerobe cannot grow at all in the presence of oxygen.
Bacterial culture on an agar plate

Sample from forearm

Sample from fingertips
What is antibiotic sensitivity testing?
Antibiotic sensitivity testing determines which antibiotics inhibit the growth of the bacteria that have been cultured. This information allows the selection of the most suitable antibiotic to treat a particular infection. Antibiotic susceptibility testing is used to determine:
- The effectiveness of particular antibiotics against particular bacteria
- Whether the bacteria are resistant to selected antibiotics
- To identify bacterial antibiotic resistance patterns.
What is a Gram stain?
A Gram stain uses a series of stains or dyes on a sample, followed by inspection under a light microscope to detect and identify bacteria as Gram-positive or Gram-negative. A Gram stain can be done on the original sample, but it is usually done on cultured bacteria after transferring a colony of bacteria from the agar plate to a glass microscope slide.
- A Gram-positive bacterium appears purple due to crystal violet dye adhering to the cell wall.
- A Gram-negative bacterium appears red, as it is counterstained with a red dye such as saffron.
The Gram stain also identifies the bacterium's shape and behaviour.
- Cocci are round in shape
- Bacilli are rod-shaped
- Some bacteria form clusters whilst others form chains

Gram stain of corynebacteria cultured from forearm skin*
*Note palisading/ paralleling of cells in 'Chinese lettering' formation
What other tests can be done with bacterial cultures?
Coagulase test
Coagulase is an enzyme produced by certain bacteria that converts fibrinogen to fibrin and is observed as clumping of cells in plasma. The coagulase test differentiates coagulase-positive Staphylococcus aureus from coagulase-negative staphylococci.
Catalase test
Catalase is an enzyme that degrades hydrogen peroxide into hydrogen and oxygen. The bacterial sample is added to a test tube of hydrogen peroxide. The production of bubbles (oxygen) indicates a positive result. The catalase test differentiates catalase-positive staphylococci and micrococci from catalase-negative streptococci.
What blood tests are done in bacterial infections?
Blood tests require a sample of blood accessed by a needle from a vein. Examples of those requested for bacterial infection include:
- Full blood count —a bacterial infection often raises the white cell count with neutrophilia
- C-reactive protein (CRP) — this is elevated above 50 in serious bacterial infections
- Procalcitonin — a marker of generalised sepsis due to bacterial infection
- Serology — tests 10 to 14 days apart to determine immune response to a particular organism
- Rapid Plasma Reagin (RPR) test (and others) — if syphilis is suspected
- Blood culture — if high fever > 38°C.
Polymerase chain reaction (PCR)
PCR involves isolating and amplifying lengths of bacterial DNA from a sample of skin, blood or other tissue. The DNA is compared to bacterial DNA from known organisms, thus identifying the species. It is useful for slow-growing bacteria such as anaerobic bacteria and mycobacteria (tuberculosis and atypical mycobacteria), as these cannot be cultured by standard methods.
Enzyme-linked immunosorbent assay (ELISA)
ELISA can test for specific organisms either by detecting bacterial antigen during an infection or antibacterial antibody. The detection of the antibody confirms contact with an organism at some time but it is not necessarily the reason for a current infection.
ELISA is rarely used for the detection of skin bacteria. It may be used to detect:
- Borrelia burgdorferi in Lyme disease
- Treponema pallidum in syphilis.
References
- Aly, R. Microbial Infections of Skin and Nails. Chapter 98. Medical Microbiology. 4th Edition. University of Texas Medical Branch at Galveston. 1996.
- Lazarus JJ, et al. ELISA-based measurement of antibody responses and PCR-based detection profiles can distinguish between active infection and early clearance of Borrelia burgdorferi. Clin Dev Immunol. 2012; 2012: 138069. PubMed
- Medscape. Bacterial wound culture. Lemuel R Non, MD
On DermNet
- Bacterial skin infections
- Staphylococcal skin infections
- Streptococcal skin infections
- Impetigo
- Laboratory tests for fungal infections
- Laboratory tests for viral infections
- Bacterial infections online course for health professionals
- Blistering skin conditions
Other websites
- Bacterial infections of the skin — DermNet e-lecture [Youtube]
