Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Mycosis fungoides pathology — extra information
Lesions (cancerous) Diagnosis and testing
Mycosis fungoides pathology
Author: Adjunct A/Prof Patrick Emanuel, Dermatopathologist, Clinica Ricardo Palma, Lima, Peru. DermNet Editor-in-Chief: Adjunct A/Prof Amanda Oakley. Copy edited by Gus Mitchell. July 2018.
Introduction Histology Special studies Differential diagnoses
Introduction
Mycosis fungoides is the most common form of cutaneous T cell lymphoma. It is characterised by infiltrates of lymphocytes and an indolent clinical course, usually slowly progressing from patches to thicker plaques and eventually to tumours.
Histology of mycosis fungoides
In mycosis fungoides, the histopathology is characterised by infiltrates of malignant T-cells. These are small to medium in size, and characteristically have irregular cerebriform nuclei. The clinical stages (patch, plaque, tumour) correlate with the progressive density of malignant T-cells.
Patch stage mycosis fungoides: there is a superficial lichenoid infiltrate, mainly of lymphocytes and histiocytes and a few atypical cells infiltrating the epidermis without significant spongiosis (a phenomenon which is known as 'exocytosis', figure 1). This stage may be very subtle histopathologically and mimic other dermatoses such as eczema or lichenoid dermatoses, as the atypia may be difficult to appreciate. Often multiple biopsies are required to make the diagnosis and numerous studies may be needed to isolate or prove a clonal proliferation of T-cells.
Plaque stage: as mycosis fungoides progresses, there is more obvious epidermotropism (figure 2) and a denser dermal infiltrate. There may be intraepidermal collections of atypical cells (Pautrier microabscesses, figure 3).
Tumour stage: when tumours start to form clinically, histopathology shows a much denser dermal infiltrate (figure 4). There may be no exocytosis of lymphocytes in this stage. Transformation to large cells may occur (figure 5).
There are numerous clinical and histopathological variants of mycosis fungoides including a folliculotropic variant (figure 6), a granulomatous variant (granulomatous slack skin syndrome), and variants that mimic common dermatoses such as pigmented purpuric dermatitis and vitiligo.
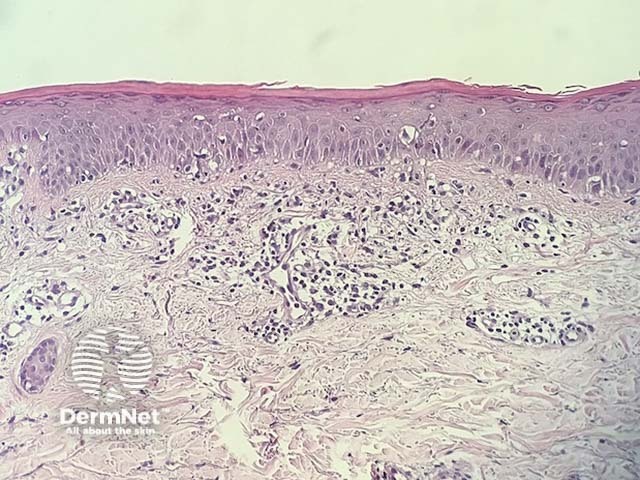
Figure 1
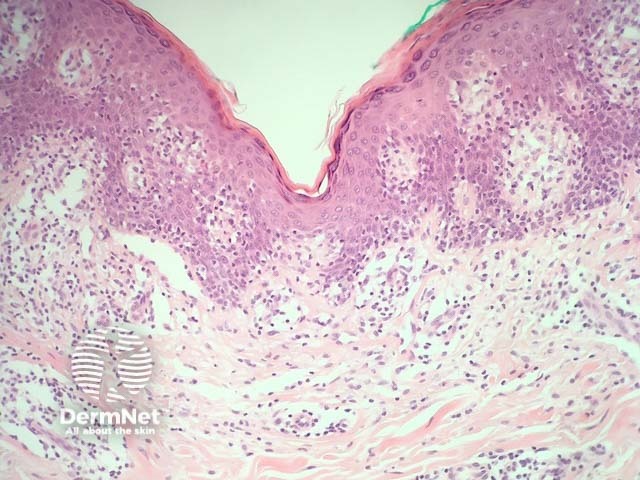
Figure 2
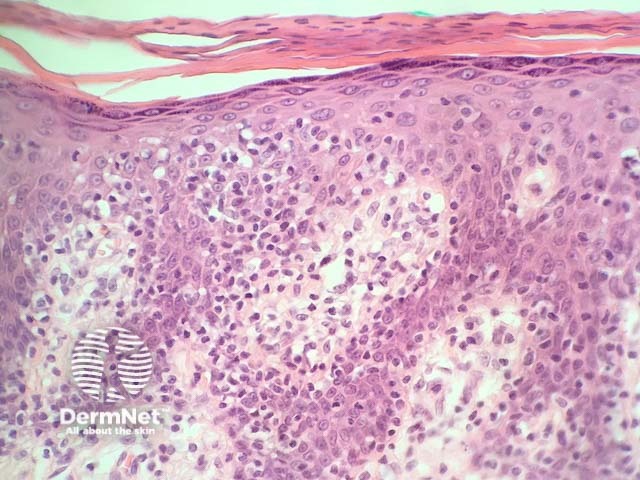
Figure 3
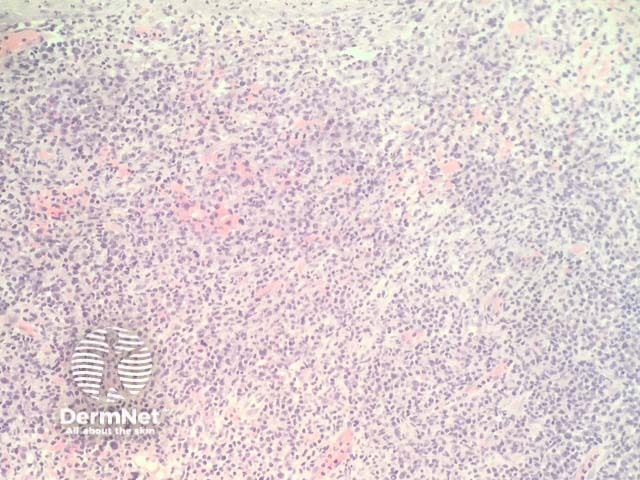
Figure 4
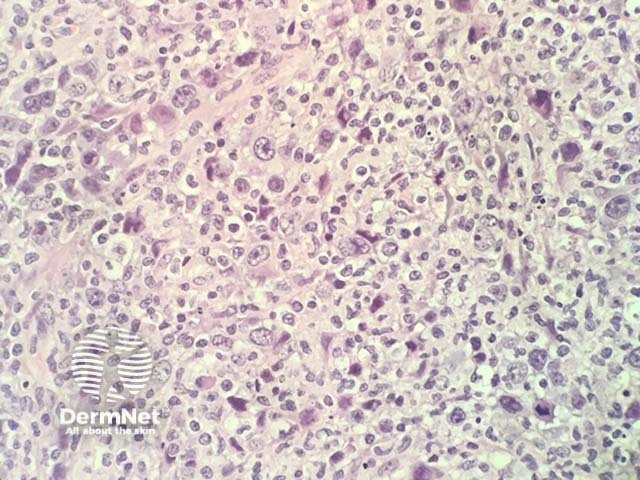
Figure 5
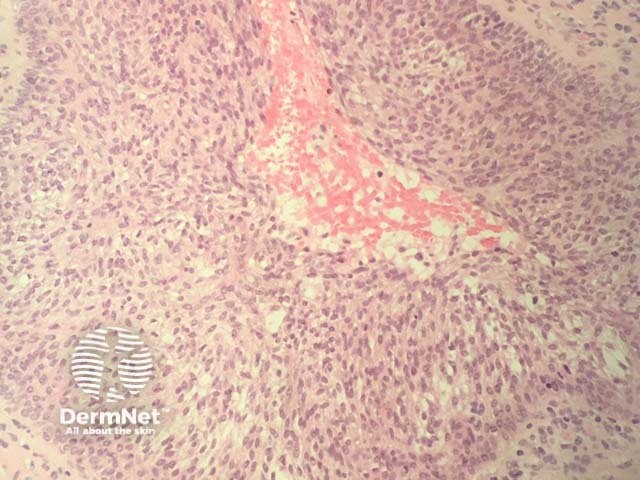
Figure 6
Special studies for mycosis fungoides
In challenging cases it can be useful to prove the presence of clonal proliferation of T-cells to make the diagnosis. This can be done with immunohistochemistry and T-cell gene rearrangement studies.
Immunohistochemistry: Mycosis fungoides usually shows a predominance of CD4+ T -ells with fewer CD8+ cells (though CD8 variants do exist). The ratio of CD4/CD8 can be assessed and if there is restriction of one type this would indicate evidence of clonality. CD4 can also be useful to highlight the degree of T-cell infiltration into the epidermis. Clonal T cells also often lose T-cell marker; malignant T-cells a sometimes negative for CD7 and CD5.
T-cell gene rearrangement studies demonstrate a clonal population of T-cells in the majority of cases
The differential diagnosis for mycosis fungoides
Other diagnoses to be considered include:
- Dermatoses psoriasis, eczema and lichenoid dermatoses can all mimic mycosis fungoides. Sometimes multiple biopsies, careful clinical correlation, and special studies are needed to secure the diagnosis of mycosis fungoides
- Other cutaneous lymphomas — numerous other lymphoproliferative disorders can mimic mycosis fungoides histologically. Sézary syndrome, CD8+ cytotoxic aggressive T cell lymphoma, and the mycosis fungoides-like form of lymphomatoid papulosis (type B) are particularly close mimickers and need correlation with the clinical presentation to exclude
- Vitiligo — early inflammatory phases of vitiligo can mimic mycosis fungoides. This is particularly problematic in cases of hypopigmented mycosis fungoides. Correlation with special studies can be particularly helpful in these cases.
References
- Yamashita T, Abbade LPF, Marques MEA, Marques SA. Mycosis fungoides and Sézary syndrome: clinical, histopathological and immunohistochemical review and update. Anais brasileiros de dermatologia 2012; 87(6): 817–30. doi:10.1590/S0365-05962012000600001. PubMed
On DermNet
- Cutaneous T cell lymphoma
- Mycosis fungoides images
- Sézary syndrome
- Mycosis fungoides palmaris et plantaris
- Dermatopathology glossary
- Dermatopathology index
